Today, we're diving deep into Women's Health in order to answer life's greatest mystery: How Did Women Manage Their Periods Back in the Day?
In order to define what is "Back in the Day", we have to uncover when Pads and Tampons were invented. Note that Menstrual Cups is a more recent invention that is gaining popularity and traction, but more on that mystery and "conspiracy" another time.
After a quick Google search, I discovered that sanitary pads were first developed in 1888 by nurses mending to the wounded on the battlefield. The nurses wanted to create a pad that was super absorbent, in order to help stop the soldiers from bleeding.
The concept of the pad didn't catch on until much later due to various reasons like comfort, price, and embarrassment. It actually wasn't until the 1980's that pads with wings were invented to improve the fit and comfort. Unfortunately, pads can still be expensive, especially for those in Third World Countries.
So, now that we have a 1888 as the benchmark for when sanitary pads were invented, we can do another quick Google search into what women used and did before 1888.
According to Femme International, pads were mentioned in the "10th century in Ancient Greece", and it seemed as though rags were used.
And according to Owlcation, "Prior to the 20th century, European and American women menstruated infrequently compared with today", in which they explained that women weighed less then than today, which is the cause for this phenomenon.
However, women still menstruated, so they had to use various items from "grass, rabbit skins, sponges, rags, menstrual aprons, homemade knitted pads, or other kinds of absorbents". See! Rags is mentioned again, so we can assume that rags were common place since Ancient Greece till the Industrial Era.
Then Owlcation mentioned that "Menstrual huts... were a place where women separated from the community during their menses for various reasons ranging from fear to respect". Hmmm... what does a menstrual hut look like?

Pictured is menstrual hut in Nepal. This tells us that even in 2022, there are people in some countries that don't have access to disposable pads, and continue to stay in these menstrual huts.
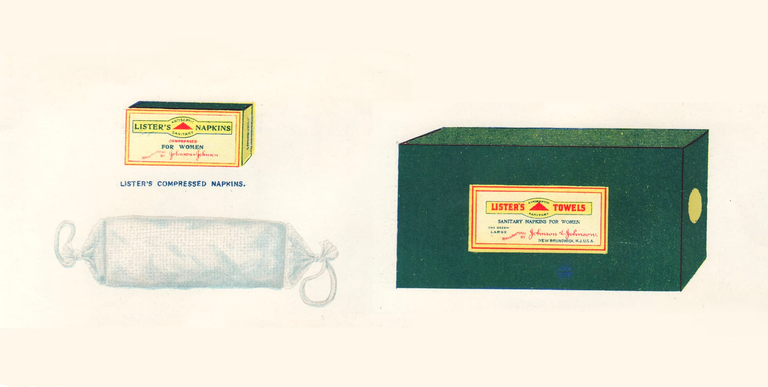
Owlcation continues with the invention of the disposable pad, saying, "Johnson & Johnson's sanitary napkins were said to be the first commercially available disposable sanitary protection products for women in the United States. The earliest ones the Company sold were called “Sanitary Napkins for Ladies” and “Lister’s Towels”.
Wow! So one of the inventors of the Johnson & Johnson COVID-19 vaccine, ALSO created the modern day sanitary napkin. That's pretty interesting.
I remember watching a show on Netflix, called, "Period. End of Sentence", and it was a profound documentary about how women in India are trying to normalize periods and fight for having disposable pads. It is a sobering reminder of how lucky we are to be living in more affluent places.
Here is where you can view the Netflix documentary.
The question begs, why exactly do women have periods the way they do now?
Modern medicine textbooks state that women have a cycle every 28 days... and that's just those with a normal menstrual cycle. So, we will deep dive into female anatomy to understand why women bleed every month - which is the whole reason why this article was written in the first place. Below will be heavier on women's health if you'd like to continue:
Breasts
- When girls develop breasts buds, that is the start of puberty
- When breast buds form, it is typical for the buds to be asymmetric
- BRCA1 or BRCA2 gene mutation contributes to a very high risk for developing breast cancer, which can be confirmed with tissue biopsy
Cervix
- Essentially, the entrance to the uterus, and the site for Papsmear sample collection
- Bright-red bumpy tissue called a cervical ectropion can develop - benign finding, but makes the cervix more friable or easier to bleed
- Birth control pills may contribute to larger ectropions due to higher estrogen levels
- Good practice to sample the ectropion during a Papsmear
Mucus of the Cervix and Vagina
- Can be dry, thick white, runny white, and clear and stringy
- Can sometimes be mixed with blood
Uterus
- Fibroids known as uterine leiomyoma or myoma can enlarge the uterus, which can cause heavy menstrual bleeding called menorrhagia, pelvic pain or cramping, and bleeding between periods
- Fibroids are usually benign, except for the heavy bleeding, and is rarely malignant
Ovaries
- Produce estrogen, progesterone, and a little bit of testosterone aka androgens
- Polycystic Ovary Syndrome (PCOS) makes prone multiple cysts on the ovaries and high androgen levels, which lead to acne, body hair aka hirsutism, oligomenorrhea, and resistance to insulin.
- During menopause, ovaries atrophy. Ovaries should not be palpable during a bimanual exam. If palpable, order an intravaginal ultrasound and refer to a gynecologist.
Menstrual Cycle
- typically lasts 28 days
- Remember back to my Endocrine Article? If not, all you need to know is that the hypothalamus in your brain sends hormones to your anterior pituitary that is located inferiorly, but also on the brain, which then sends other hormones i.e. FSH and LH to the target organs - in this case, the ovaries and uterus.
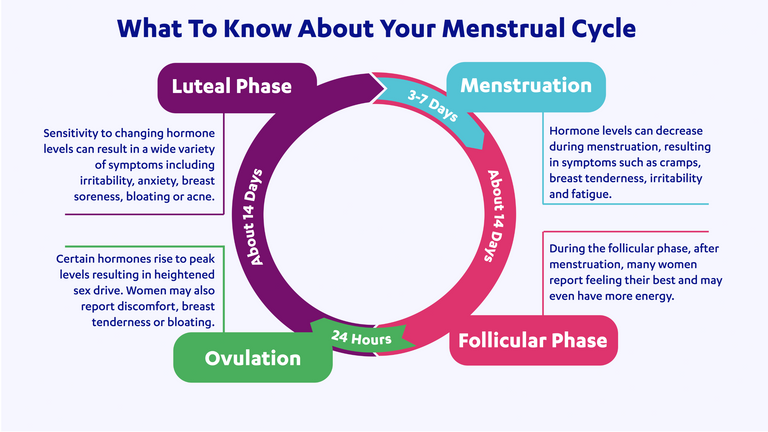
Follicular Phase aka Proliferative Phase - Days 1 - 14
- During the first 2 weeks of the menstrual cycle, estrogen takes center stage.
- Estrogen stimulates the development of the endometrial lining in the uterus.
- Follicle Stimulating Hormone (FSH) from the anterior pituitary stimulates the immature eggs aka follicles into producing estrogen.
Midcycle (Day 14) - Ovulatory Phase
- Luteinizing hormone (LH) is secreted by the anterior pituitary, which induces ovulation of the follicles.
- The follicle travels to the fallopian tube.
Luteal Phase (Days 14 to 28)
- Progesterone takes over as the dominate hormone during the last 2 weeks of the menstrual cycle.
- The corpus luteum produces progesterone, which stabilizes the endometrial lining.
Menstruation
- If no pregnancy occurs, then both estrogen and progesterone will decline, which induces menses or bleeding.
- Low estrogen and progesterone levels trigger the hypothalamus to signal the anterior pituitary to produce FSH, which starts the cycle over again.
Fertile Time Period
- Sexual intercourse during days 1-2 before ovulation offers the highest chance of pregnancy
- Noted copious clear mucus that feels thin and elastic in the vagina - sign used in the Cervical-Mucus Method of birth control.
- Can use ovulation kids purchased over the counter (OTC) to detect urinary LH, which if you remember is Midcycle (Day 14), that indicates ovulation.
- False positive results are possible with women with PCOS, ovarian insufficiency, and menopause.
Now that we have an understanding of the phases of the menstrual cycle... ahem, NORMAL menstrual cycle, we have to also understand reasons why menstrual cycles can be abnormal. Reasons are many, and can range from fibroids to pregnancy.
Dysmenorrhea
- Painful periods due to severe menstrual cramps, caused by high levels of prostaglandins
- Treat with NSAIDs, such as ibuprofen, and heating pads
Amenorrhea
Primary amenorrhea
- No menarche by age 15; 50% of cases caused by Turner syndrome
- Turner's Syndrome happen in females with complete or partial absence of the second sex chromosome X (Remember females are XX, and males are XY) - can lead to lymphedema, webbed neck, high-arched palate, short fourth metacarpal, short stature, ovarian failure, cardiovascular and renal issues, ear malformations, and other health problems.
- Puberty is delayed if there is no breast development by age 13, no pubic hair by age 14, and no menarche by age 15
Secondary amenorrhea
- No menses for three cycles or for 6 months
- Most common cause is pregnancy, but other causes can be ovarian, stress, anorexia, or polycystic ovary syndrome (PCOS)
- can be associated with exercise and being underweight i.e. excessive exercise or sports or calorie deficiency
- "female athlete triad" - anorexia, amenorrhea, and osteoporosis
So how do we test for irregularity? It ranges from lab tests to examination and a biopsy of the cervix and uterus.
Labs associated with testing for irregularity and amenorrhea are: pregnancy test, serum prolactin level to rule out prolactinoma-induced amenorrhea, serum TSH, FSH, and LH. If amenorrhea has been going on for more than 6 months, check bone density.
Examination for irregularity is a little more invasive, and involves:
The Bethesda System
- Standardized system used for reporting cervical cytology (Pap test) results.
- Combined with human papilloma virus (HPV) testing is used to screen for cervical cancer.

ASC-US: Atypical Squamous Cells of Undetermined Significance
- 20 y.o. or younger - repeat Pap in 12 months
- 21 to 24 y.o. - repeat Pap in 12 months
- 25 to 29 y.o. - reflex HPV test, but can repeat Pap in 12 months
- 30 y.o. or older - positive cancerous HPV (typically type 16 and 18), refer to colposcopy - if that HPV is negative, then co-test in 3 years
AGCs: Atypical Glandular Cells
- Associated with premalignant or malignant cases
- Refer for endometrial biopsy
LSIL: Low Grade Squamous Intraepithelial Lesions
- cervical cells show changes that are MILDLY abnormal, typically from HPV infection
- 21 to 24 y.o. - repeat Pap in 12 months
- 25 to 29 y.o. - refer to colposcopy with cervical biopsy
- 30 y.o. and older - repeat Pap test or colposcopy in 12 months, but if HPV positive, then refer for colposcopy with cervical biopsy
HSIL: High-Grade Squamous Intraepithelial Lesions
- associated with precancer and cancer
- 21 to 24 y.o. - refer to colposcopy with cervical biopsy
- 25 y.o. - refer for immediate excisional treatment, typically by loop electrosurgical excision (LEEP) or cervical conization surgery
Reflex HPV Testing (HPV DNA test)
- HPV 16 and 18 cause 70% of all cervical cancer cases.
- Vaccines, Gardisil (indicated for both male and female) and Cervarix (only for females), are approved for ages 9 - 26 y.o.
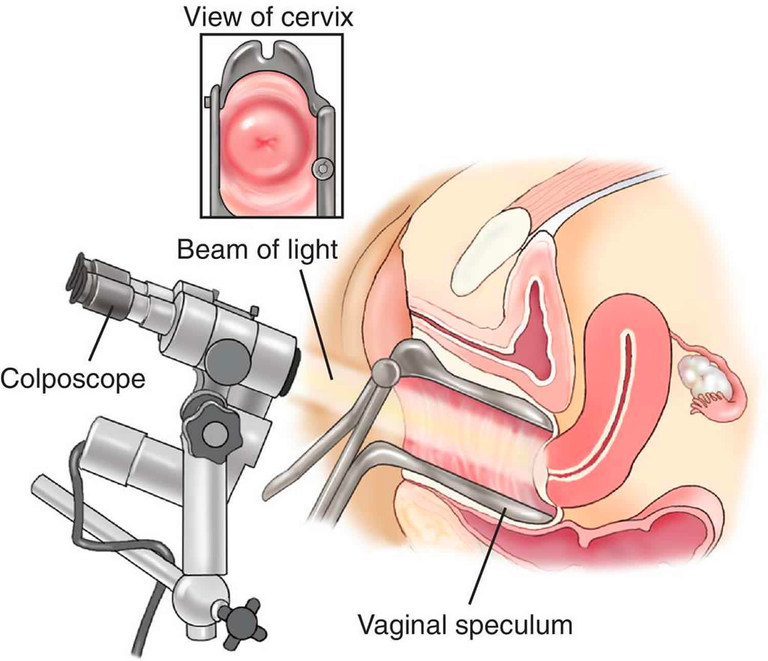
Colposcopy - specialized microscope to view the cervix
- biopsy of the cervix can be obtained during a colposcopy
- vaginal speculum is used to view the cervix, and then the cervix is washed with 3-5% acetic acid aka vinegar, which removes mucus, and causes abnormal regions to turn bright-white.
- after biopsy and colposcopy is done, cramping and spotting is expected for the next few days
Loop Electrosurgical Excision Procedure (LEEP)
- device used like a scalpel to cut through the cervix (conization) to treat cervical cancer
- if the lesions are mild, cancerous cells can be removed by cryotherapy, laser ablation or surgical conization
Potassium Hydroxide Slide
- vaginal specimens are placed on a slide, and potassium hydroxide (KOH) is dropped onto the specimen to visual under a microscope to view hyphae and spores (evidence of fungal infection)
Whiff Test
- Bacterial Vaginosis (BV), which is NOT an STI, emits a strong fishy odor, which is released on the slide by dropping KOH on it - will see clue cells
Tzanck Smear
- Evaluates herpetic infections - positive will show large abnormal nuclei in squamous cells
Now, if you didn't know much about women's health before this article, you should have a pretty good understanding of it now. Women's health is complicated... they have to go through so much!
Obviously, there is a lot more I'd like to go into, but I shall save it for another article. Join me on my continuing series on the Mysteries of Health and Care.