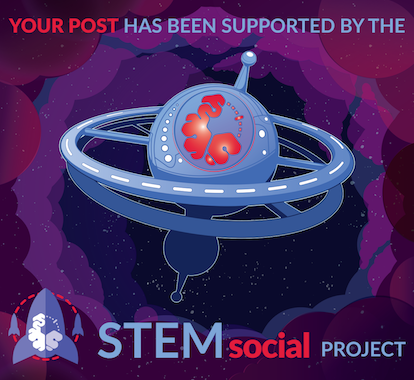
By Myupchar, CC BY-SA 4.0, Wikimedia
In this post, we will look at the various presentations of indigestion, the causes, and what can be done.
CLINICAL PRESENTATION OF DYSPEPSIA
Persons who have dyspepsia commonly experience upper abdominal discomfort, burning sensation in the stomach, bloating, belching, feeling of fullness, early satiety, regurgitation, heartburn, etc. These symptoms cause a lot of discomforts and in some cases, they may be recurrent.
CAUSES OF DYSPEPSIA
As I stated in the introduction, the causes of indigestion can be functional (non-ulcer dyspepsia) or pathologic.
For the functional causes, there is no underlying anatomical abnormality in the digestive system, that is, there is no obvious cause for the symptoms. This occurs due to the intake of food which irritates the stomach lining (food allergies), dysfunctional relaxation and emptying of the stomach, nervous system dysfunction, Helicopter pylori infection, etc.
Functional dyspepsia is more commoner in females. Other risk factors include chronic use of over-the-counter medications like some pain relievers which can irritate the stomach lining, psychological stress, smoking, depression, etc.
The pathologic causes of dyspepsia include; Peptic ulcer disease, Gastroesophageal reflux disease (GERD), Gastric carcinoma, gastritis, Zollinger-Elisson syndrome, and others.
Peptic Ulcer Disease (PUD) and Gastro-esophageal Reflux Disease (GERD) are part of the acid peptic disorders in which gastric acid and pepsin are the causative factors. They are the most common causes of dyspepsia with underlying etiology. We will discuss the two of them one after the other.
PEPTIC ULCER DISEASE (PUD)
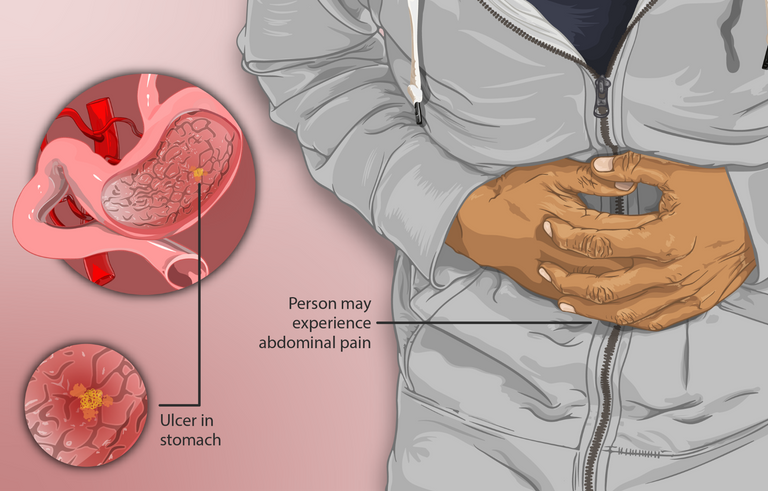
Peptic ulcer disease occurs when there is a break in the inner lining (mucosa) and submucosa of the stomach or duodenum thereby forming an open sore. PUD results from an imbalance between the protective and aggressive factors on the inner lining of the stomach and duodenum.
By BruceBlaus - Own work, CC BY-SA 4.0, Wikimedia
Normally, the stomach and duodenum have some factors which constitute an injury to their inner lining. As well, they also have factors that help to protect the inner lining from these injuries.
These aggressive and protective factors exist in a balance to maintain a normal mucosa lining. However, when there is an imbalance, and the aggressive factors now overpower the protective factors, then the aggressive factors begin to injure the mucosa lining and the sub musosa. This results in an ulcer.
The aggressive factors include gastric acid which has a corrosive effect on the mucosa lining, Pepsin and pancreatic enzymes which have a proteolytic effect, and bile salts which dissolve the cell membranes of the epithelium.
The protective factors include a mucus layer that serves as a lubricant on the epithelium, the bicarbonate system which maintains acid/base balance, and the tight junctions of the epithelium. These factors help to protect the epithelium from the aggressive factors mentioned above.
When the aggressive factors overpower these protective factors, injuries (ulcers) result.
Peptic ulcer occurs in the stomach (gastric ulcer) and the duodenum (duodenal ulcer). It can also occur in the esophagus and the jejunum.
Gastric and duodenal ulcers may have a common presentation but there exist some clinical differences.
Duodenal ulcers have a younger age of onset (25 - 75 years) while gastric ulcers have an older age of onset (55 - 65 years). Duodenal ulcers are commoner in females and less associated with malignancies while gastric ulcers are more associated with malignancies and are relatively more difficult to treat than duodenal ulcers.
CAUSES OF PEPTIC ULCER DISEASE
The two most common etiologies of peptic ulcer disease are Helicobacter pylori infection and chronic use of pain drugs (NSAIDs). Other rare causes include viral infections, G cell Hyperplasia, Zollinger-Elisson syndrome, etc.
DIAGNOSIS AND TREATMENT OF PUD
Diagnosis of PUD is made using the clinical features together with some laboratory investigations. Some important laboratory investigations include urea breath test to check for H. Pylori, stool antigen tests, serology, etc.
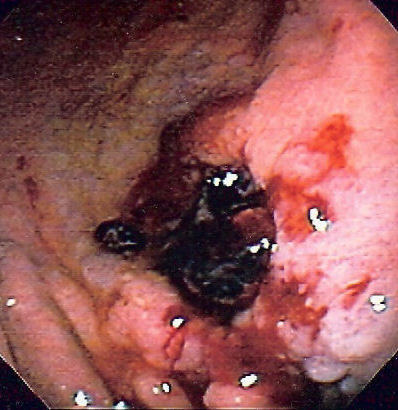
Another important diagnostic investigation is the upper gastrointestinal endoscopy. In this investigation, a tube with a camera is passed through the esophagus into the stomach and upper part of the duodenum. The camera visualizes the gastrointestinal tract and displays the ulcers and their features on the screen.

By Samir - Own work, CC BY-SA 4.0, Wikimedia
The treatment of peptic ulcer disease is usually through a triple regime using a proton pump inhibitor (PPI), and antibiotics (Clarithromycin, Amoxicillin, or Metronidazole).
COMPLICATIONS OF PUD
Apart from dyspepsia and other discomfort caused by peptic ulcer disease, there can also arise some complications if left untreated.
One of the major complications is bleeding. The ulcer can be bleeding internally and the patient may be losing blood gradually without knowing.
The ulcer can also eat the wall of the stomach or intestine deeper and deeper till it perforates. On perforation, the contents of the stomach or duodenum are then poured into the sterile peritoneum leading to peritonitis which is a very serious and life-threatening condition.
PUD can also obstruct the stomach outlet leading to gastric outlet obstruction and stasis of food in the stomach.
The ulcer can also have a malignant transformation, especially gastric ulcers.
CC BY-SA 3.0, Wikimedia
So to avoid these complications, those who have ulcers should ensure to see a doctor and get adequately treated and as well as follow the lifestyle modifications that will be prescribed by the doctor.
GASTRO-ESOPHAGEAL REFLUX DISEASE (GERD)
GERD is another cause of dyspepsia which occurs when there is abnormal relaxation of the lower esophageal sphincter. This causes the backflow of gastric contents into the esophagus.
Normally, when we swallow food into the stomach, it does not come back to the mouth or esophagus (the tube that connects the mouth to the stomach). This is because there is a band-like structure at the junction between the esophagus and the stomach which prevents the backflow of the contents of the stomach into the esophagus and the mouth.
However, when this band-like structure becomes lax or faulty, it now allows a backflow of the contents of the stomach into the mouth. This is called Gastroesophageal reflux disease.
The symptoms are dyspepsia, regurgitation, difficulty or painful swallowing, heartburn, burning upper abdominal pain, a sour substance in the mouth, etc.
COMPLICATIONS OF GERD
This disease is also associated with some complications, the most significant is the barret esophagus.
Because the content of the stomach is acidic and the esophagus was not made for acidic contents, continuous backflow of the acidic contents of the stomach into the esophagus, overtime denatures the cells of the esophagus which cannot withstand the acidic nature of the stomach contents. This is referred to as the barret esophagus.
TREATMENT AND LIFESTYLE MODIFICATIONS IN GERD
The drugs used for the treatment of GERD are drugs that lower the acidic contents of the stomach like Proton pump inhibitors and H2 receptor antagonists.
However, a very important aspect of the management of GERD is lifestyle modification.
A patient with GERD should always sleep with the head elevated with a pillow. This is to avoid micro aspirations which are dangerous to the lungs. It also helps the food to gravitate towards the stomach and not flow back to the esophagus.

By Alexey Venetsianov, Public Domain, Wikimedia
It is also helpful to always eat dinner early and stay up at least 2 hours before lying down. The patient should also avoid some foods like carbonated drinks, fried foods, alcohol, etc. It is encouraged to eat bit by bit and avoid overfeeding.
Those who are overweight are also encouraged to lose some weight. Most importantly, take a lot of water, fruits, and vegetables and stay healthy.
Thanks so much for reading. A happy new week to you all.
For further reading and inquiries, please check the links below:
American Academy of Family Physicians