So this post is just a addendum to the post made by one of my new mentee. After critically reading the post and from comment made about it as regards how difficult it was to comprehend, I have decided to make the concept less cumbersome and easy to understand. I believe with time she will perfect her writing skills.
It's going to be a short but impactful read and my focus will simply be to explain in details why there are challenges associated with neonatal blood transfusion.
Already, she has made some explanation on what neonates are and some of the circumstances surrounding the possibility of the cross matching in neonates. My main aim here is to elaborate more about the cross matching which is different from the regular one done with adults.
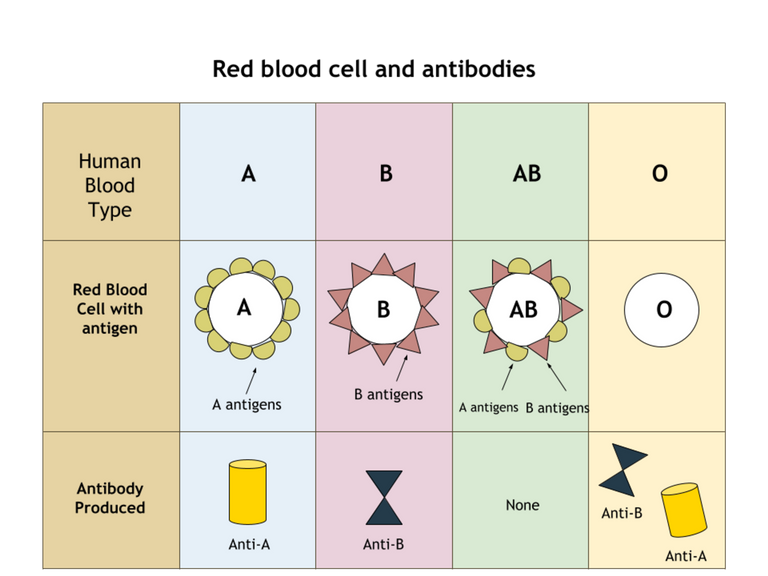
Just for reference sake, neonates are simply newborns less than 4 weeks old. To make it clearer, all our blood groups (A, B, AB and O) are already formed even before birth but when it comes to antibodies, the case is different. Neonates do not have their own antibodies rather they have that of their mother circulating in them (maternal antibodies).
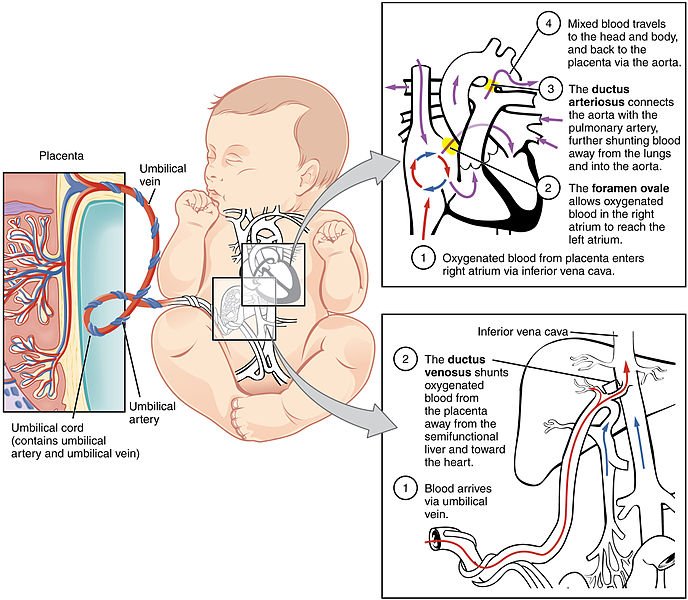
A greater percentage of the blood in neonates are from the mother since their bone marrow cells are yet to be fully matured and functional. Moreover, all the while they were in the uterus, they have been receiving blood supply from the mother.
If you would recall, we have critically discussed cross matching in some of my previous post. Just to make it easier, cross matching involves the reaction between a donor's red blood cells (contains the antigens) and a recipients serum (contains the antibodies). In summary, the red blood cells contains the antigens while the serum contains the antibodies.
A reaction between an antigen and antibody to form what is known as agglutination (a visible clump) is indicating that the reaction is positive and simply means that the blood is not compatible. When there is no visible reaction or clumps, then we say the blood is compatible. This is simply the basic principle underlying Cross matching.
Naturally, antibodies are produced against antigens and they are found mostly in serum or plasma, but mostly, you have higher concentration of them in the serum. Antigens reside mostly in blood and the red blood cells have antigens on their surfaces.
Recalling the one and simple rule by Landsteiner, you will always produce antibodies against any antigens your body lacks. For deeper understanding, You can read more about this concept here,I prepared a very easy to understand article on it.
In human developmental stage, between antigens and antibodies, antigens are the first to be produced before antibodies. Antibodies are only produced mainly after birth and it starts from 4 months of age. Since antibodies are required to do a cross match, you would not expect to see the actual antibodies of a newborn baby circulating in them, mostly, what will be in their blood circulation is that of their mother.
By circulation, we are strictly referring to their plasma. Remember we earlier established the fact that antibodies are found in the plasma or serum. To make things much clearer here, plasma is a blood components gotten when blood is collected in an anticoagulant container and allowed to settle or spun in a centrifuge.
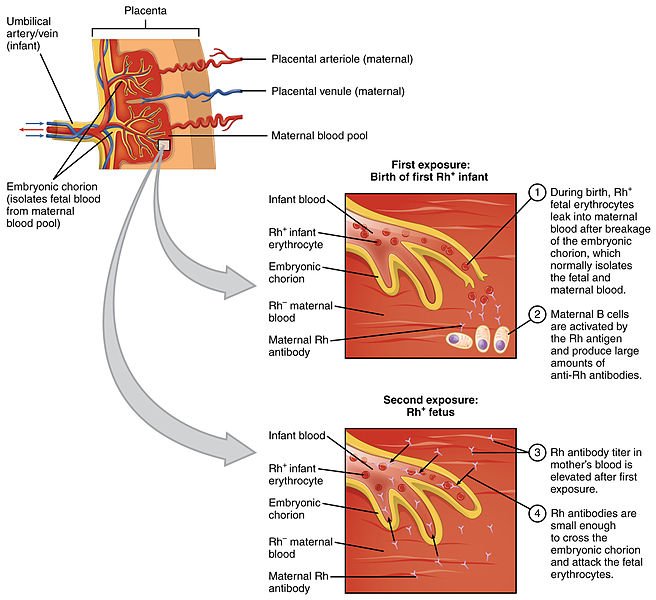
Antibodies (anti A and B) are IgG antibodies and they have the potency of passing through the placenta barrier that connects the mother to the unborn child. As they pass this placental barrier, they enter the baby's blood. If the baby's blood is not compatible with that of the mother, it can cause the mother to produce antibodies against the baby's blood, thereby leading to neonatal transfusion reaction that causes haemolysis of the baby's blood. This is commonly known as hemolytic disease of the newborn, HDN
Erythroblastosis fetalis aka HDN
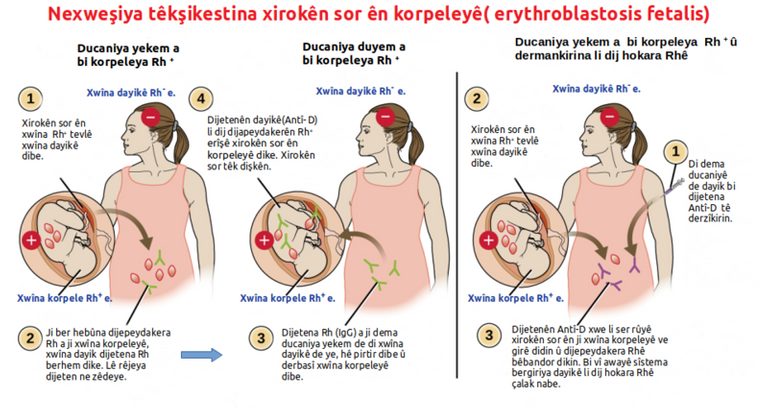
Haemolytic disease of the new born is usually seen in cases where a Rhesus negative woman (a woman who has not been sensitized to produce antibodies against human red blood cells) bears a Rhesus positive child (an already sensitized child). By virtue of the fact that their is a maternal - fetal blood circulation, a baby's blood that has already been sensitized can enter the woman blood circulation.
The body of the mother detects this as foreign and then produces antibodies against the blood (the baby's). The first child of the woman will survive this but subsequent pregnancy by the woman, fetus will be affected, if not even killed. This is because, the woman had already developed antibodies against the baby's blood and since they are IgG antibodies, they can easily pass through the placenta and enter the baby's blood to attack and destroy them. It will only take a Rhogam injection to stop this reaction from future occurrence in the woman.
What rhogam injection do is to simply mop up all the antibodies produced by the mother's and to a greater extent even prevent their formation or maturity. For antibodies to be fully formed against the baby's blood, it takes roughly about 72hours.
So by implication, if a Rhesus negative woman gives birth to a Rhesus positive child, the rhogam injection must be given to the woman within the timeframe to prevent the formation of antibodies.
Antibodies formation maternal circulation and the Inhibitory effect of rhogam injection
If the rhogam injections is not given to the woman and the antibodies are allowed to be full formed, then it remains permanent for life. Every child conceived by the woman will always either be still birth (dead babies in the womb prior birth) or jaundiced babies.
This once again reminds us of the importance of doing compatibility testing and indirect coombs test to know the blood status of a pregnant woman prior delivery. Usually, feto-maternal blood mixing occurs externally during childbirth or delivery and this is the major point the antibodies against the baby are developed.
Rhesus factor always play a huge role in the etiology of this problem. Going for antenatal testing is very important because, it is at stage that any complications that might arise at the long run will be detected.
What you will expect with neonatal cross match
Proceeding to do a cross match with the serum or plasma small collected from the neonate will give a false results because the antibodies that will likely be present does not reflect those of the baby rather, those of the mother, since they are yet to start producing antibodies.
The chances are high that, the baby will react to any blood after the cross match. It is easier to know the blood group antigens (A, B, AB, and O) of a neonates than knowing the type of blood group antibodies they have. Since cross matching is not possible, what then is the way out.
This is actually where it gets confusing but I will make it much easier to understand. Usually, cross matching is best done with the mother's serum, since we already know her blood group and the corresponding antibodies that she will have. After doing the Cross matching and it is not compatible, then the chances that transfusion reactions will occur are high.
Rather than use the neonate's blood to do the cross matching, the mother's blood is preferably used. If by chance the mother happens to be of blood group O for example, then she will obviously have antibodies A and B (remember Landsteiner's law). Invariably, the neonate will also have this same antibodies in the circulation.
Now remember that we earlier explained that neonates blood groups can be accurately known since they are formed at early stage of intrauterine life (within the uterus) but not the antibodies yet.
Should the baby have a blood group A and you transfuse the baby with blood group A blood (since you presumably used the baby's serum to do cross matching) the antibodies A inside the neonate's circulation which of course are from the mother, will attack and destroy the transfused blood donors, thereby causing severe transfusion reaction in the neonate.
How to circumvent this problem
Since antibodies are in the plasma, It is much better to transfuse the neonate packed red blood cells (red blood cells that have had their plasma content removed). Doing this alone will prevent any transfusion reaction in the neonate. Although this is mostly in case where you wish to transfuse different blood groups.
To be on a safer side, it is better to transfuse the neonate with the mother's blood. In this way, there won't be any form of issues or transfusion reactions.
In summary, neonates do not have their own antibodies yet and as such, their serum cannot be correctly used for cross matching. Antibodies in neonates are of maternal origin. To accurately get the antibodies in a newborn, it is better done after 4 months. The best blood for neonates are either packed red blood cells (from non group O donors) or the mother's blood (preferable).
Trust this has helped a lot in clarifying some grey areas in the article. Feel free to ask questions on any area you still need clarification and I will glad to explain more.
Stay awesome!
References
•Transfusion in infants
•Blood transfusion in neonates and infants
•Ward management of a neonate