Decided to share this comprehensive review I made last year on issues and health challenges bothering on the use of face mask. I had to modify this article - Demystifying the myths about nose mask; mechanism and principle of filtration I sometime wrote in 2020 and added significant details to make it suitable for academic publication. I have had the course to present some excerpts from this research work thrice to some group of medical professionals in a bid to dispute a lot of things presumed to be right and ignorantly done.
I am forced to share this here because I published it as a textbook chapter in the online textbook: http://dx.doi.org/10.22271/ed.book.1309 titled Research Trends In Medical Sciences by AkiNik publications. In essence, You will likely not find it free of charge online without having to pay for it. Well, you don't have to pay to get the full details, though you might not be able to get the full textbook, but I can make it available for you at zero cost. I am releasing everything about my chapter here for free read. Research works should be wide read and easily accessible. My chapter focused issues bothering on face mask use. I will begin with the Abstract.
Abstract
The chapter addresses the salient and overlooked key areas regarding the use of face mask, the likely health implications as well as the reported side effects associated with prolonged use of face mask by both health care workers and the general populace at large. It also emphasizes on the need for proper orientation on who, when and how to put on the face mask to ensure adequate prevention against respiratory infection such as covid-19.
Keywords: face mask, covid-19, respiratory infection, body physiology, airborne pathogens, skin reaction
Introduction
The corona virus emergence and the economic trend since the breakout of corona virus in December 2020, the use of face mask has become very important personal protective equipment for health care workers and individuals in general who are more at risk of being infected.
The use of face mask was not very rampant among the general populace not until the break out of highly contagious diseases. The first incidence in which the use of face mask was rampant was during the break out of the Manchurian plague in the year 1910 to 1911 and also the break out of the deadly influenza virus in 1918 to 1919 (Bruno J Strasser and Thomas Schlich, 2020).
The economic trend amazingly drifted and in no time, coronavirus became a major world health challenge upon its declaration by WHO in March 11, 2020 as a pandemic (WHO, 2020). The surge in the price of face mask was overwhelming. Not only was the price inflated, it became an overtly sort after commodity. Manufacturers and importers took advantage of the situation to increase the price since there was massive increase in demand. Hand sanitizers became scarce and outrageously expensive.
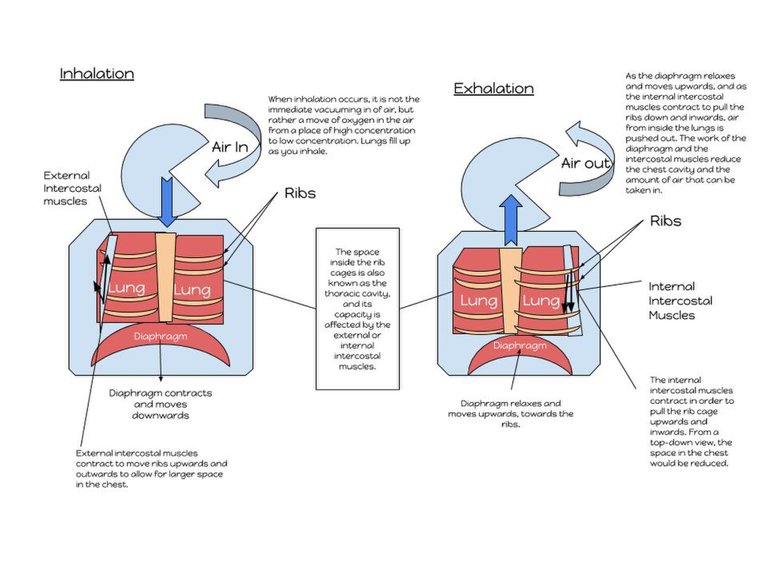
A global map of outlook of retraction and growth of Nations across the world for 2020
The whole event led to people who cannot afford them to produce locally made face mask and hand sanitizers. When critically examining the situation, one could easily conclude that, this was simply the law of demand and supply coming into play. The use of face mask has become very handy personal protective equipment (PPE) to reduce the spread of corona virus (Purushothaman, et al., 2020).
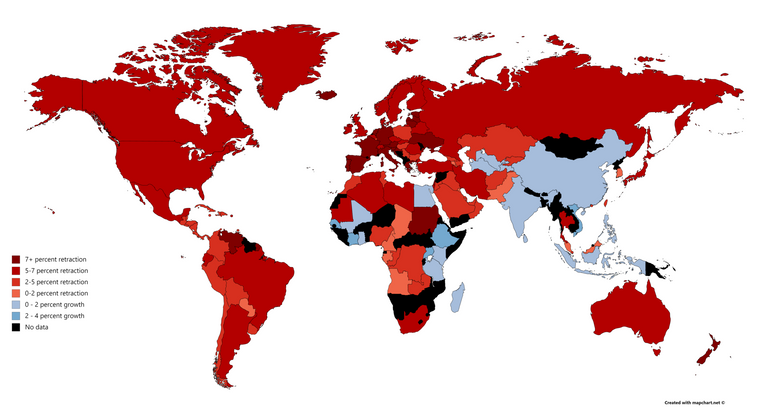
Corona virus is mostly spread through respiratory droplets and it is not air borne because is a virus that is denser than air. Respiratory droplets can be divided into two – larger droplets, usually greater than 5 micrometer (>5µm) and smaller droplets that are less than 5 micrometer (<5µm). Corona virus happens to fall under the larger respiratory droplets (Chua et al., 2020).
The implication of this is that, as they are released from the carrier when they cough, sneeze, or talk, this virus quickly settles on surfaces since they cannot travel far. Individuals get infected by touching surfaces where these viral particles have been deposited and if by chance the hand comes in contact with their mouth or nose, they become infected. As ways to reduce the spread, social distancing, washing of hands with soap and running water, hand sanitizing became important necessities.
Relative size of common airborne pathogens and contaminants
Due to the size of corona virus (60-140nm or 0.06-0.14microns), way smaller than bacteria and dust particles (Chua, 2020), they can easily penetrate any face mask that has larger pore diameter. The need to produce PPEs with pore size lesser than these pathogens becomes very essential (Tcharkhtchi et al., 2021).
As these masks are produced, the need to factor in the comfortability of the wearer or user comes into play. In an attempt to reduce the pore size of the mask to achieve efficient filtration efficiency, the ease of breathing by the user must be put into consideration. According to WHO, (2021), the three most essentials parameters that must be fulfilled before a mask is said to be in optimal performance are:
•Breathability,
•fit for use and
•effective filtration efficiency.
This has led to the production of different kinds of face
mask ranging from Surgical face mask, cloth face mask, full length face shield, filtering face piece respirators, FFRs (N95, P100, FFP2, FFP3, KN95) (Scheid, et al, 2020; Tcharkhtchi et al., 2021). The commonly used one among the FFRs in the hospital setting, is the KN95 and N95 which are non-oil proof.
The N simply is an abbreviation and stands for NIOSH, National institute for occupational Health and safety while the 95 attached to it, is the particle filtration efficiency i.e. it is able to filter about 95% of particles and aerosols of up to about 0.3 microns (300nm) thus, making it relatively efficient enough to filter the virus.
But it is worth nothing that filtration rate of face mask can also vary from one manufacturer to another (Tcharkhtchi et al., 2021). The implication here is that, the use of N95 may not guarantee total prevention from respiratory viruses like corona virus. Regardless, they offer some level of
protection when employed with adequate social distancing, hand sanitizing and frequent handwashing.
Ever since the outbreak of respiratory infections, the use of face mask became an indispensable personal protective equipment for individuals, most especially health care workers who are at the frontline of delivering health care services to sick patients. Face mask primary design
Before now, the main purpose or primary design of the face mask was to prevent the contamination of wounds and as well as to prevent any respiratory droplets from being transmitted either to or from the wearer.(Bruno J Strasser and Thomas Schlich, 2020).
The recent universal use of face mask once again announced by WHO in April, 2020 as a measure for containing and reduce the spread of the virus (Kisielinsk et al., 2020). Putting on the face mask has become a must and in fact has become a criterion before gaining access into some facility and cooperate establishment. The law was instituted as a measure to reduce person to person transmission due to possible close contact.
Since it has become imperative to put on the face mask to prevent possible transmission, the need to bring into light the likely health implication of wearing the face mask is
very crucial at this point.
Possible health implication overview
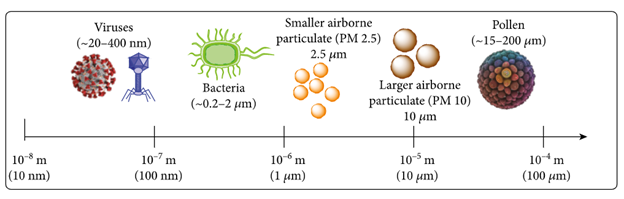
The need to draw a clear distinction between why we need to wear the face mask, how long it has to be worn, when and where, what type must be worn and how to wear them is very important. Face mask generally causes decreased air flow and permeability through the human nose which act as the primary route through which respiration occur. On the average, the nose due to its physiologic structure offers about 50% resistance to breathing (Purushothaman et al., 2020) and by implication, any further resistance to this by any means could cause potential health problem if left unattended.
Humans naturally breath in a way that could hamper on their health, the addition of obstruction in the form of face mask only makes the situation more worrisome. Thus the need for a critical study and evaluation of the possible dangers associated with the prolonged use of face mask.
The human nose primarily performs the function of filtering dust particles as well as allowing the smooth exchange of exhaled and inhaled air while breathing. The surface area is structured in such a way as to allow adequate ventilation and airflow through the nasal orifice. It is worthy of
note that the nasal orifice is made up of cilia that function optimally in moist condition and they primarily ward off dust particles as they beat in an antiperistaltic manner.
They stop functioning when the environmental condition becomes unfavourable and this is obtainable at temperature above 25 degrees centigrade and this has been attributed to continual and prolonged use of nose according to the report by (Purushothaman et al., 2020 and Kisielinsk et al., 2021).
In essence, this is a health concern that must not be overlooked and when we are talking about the use of face mask for a prolonged period of time, the risk/benefit ratio has to be put into consideration. Some individuals could have underlying health condition that may be triggered by the use face mask. The CDC, (2021) and WHO, (2020) explained in detailed the various condition and circumstances in which the face mask should and should not
be worn.
Kao, (2004) reported a clinically significant decrease in the partial oxygen pressure, increased respiratory rate and increased chest discomfort in patients wearing N-95 mask undergoing dialysis due to end stage renal disease and this is also in accordance with the report found in (Kisielinsk et al., 2021). This goes to say that, wearing of face mask actually has some potential effects on individuals even though it is not very obvious since the body health system is not compromised.
When comparing the effectiveness of different types of face mask, especially surgical and N- respirators in protecting individuals against most severe acute respiratory infection, most importantly the health care providers. The systematic review and meta-analysis reported by Smith et al., (2016) showed that, there is actually not much of a statistical significant difference between the two even though N-95 is more efficient in filtering particles.
This could be one of the reason why reinfection is observed in some health care workers. Adding more to this fact is also the general discomfort that is associated with wearing the face mask and as a result, there is more tendency of continuous touching and adjustment of the face
mask.
The partial oxygen and carbon dioxide elevation due to face mask use; a fact or a myth?
As humans’ breath naturally, gaseous exchange (carbon dioxide exchange and oxygen) occurs uninterrupted but the use of face mask may impede the proper exchange of this gas. Though this all depends on the type of face mask and the type of material from which it was made (Guo, YP et al., 2008). A cloth mask for example is a lose fitting type of mask, thus may not necessarily have much effect on the level of carbon dioxide in breathing because CO2 molecules are very small enough to escape through the mask (CDC, 2021) but this cannot be confidently said for tight fitting mask and respirators with no valves for easing breathing and also expelling exhaled air.
Carbon dioxide (C02) is a non-volatile gas that is released basically through breathing and research has shown that it has statistically significant effect by causing an increase in its concentration when the face mask is worn for a prolonged period of time (Scheid et al., 2020).
Increased partial pressure of CO2 and oxygen (O2) level in patients used for study by Rebmann et al., (2013), were reported to be increased but why they were not clinically relevant is based on the fact that, the increase was
still within the normal range of <45mmHg and 90-98% for CO2 and O2 respectively (Scheid et al., 2020).
The fact they were not clinically significant those not necessarily rule out the need for more research on the impact of this face mask. The values may not deviate from the normal physiological values what happens when they continue consistently over a longer period of time.
CO2 is a well-known respiratory stimulant and its increased retention or rebreathing due to the resistance offered by the face mask (case in point N-95), can induce increased breathing thus leading to increased respiratory muscle use (Kisielinsk et al., 2021). Besides increased muscle use, it also causes hypercapnia and increased heart rate (Cummins et al., 2020).
Constant elevation of CO2 without a commensurate decrease in its concentration by increased breathing and intake of oxygen could reduce the pH of the body system resulting to acidaemia. Tight fitting mask like the respirators cause inadequate ventilation as well as increased levels of carbon dioxide (CO2) which is referred to as hypercapnia. CO2 is a well-known respiratory stimulant, when there is a buildup of exhaled CO2 between the mask and face, this will cause an increase in lung ventilation and respiratory activity (Rosner, 2020).
H2O + CO2 ——— H2CO3 ——— H+ + HCO3-
The homeostatic mechanism of the body system is champion by
physiologic buffers that tries to maintain a balance in ph. Failure of the buffer system results to what is referred to as homeostatic disorder and one of which is respiratory acidosis which is due to insufficient clearance of CO2.
There may not be enough substantial evidences and reports so far to fully support or refute any claim that face mask causes any form of homeostatic disorder (respiratory/metabolic acidosis and respiratory/
metabolic alkalosis) because the filtration and absorbing capacity of face mask largely depends on the pore diameter as well as the material from which it was made (Guo, YP et al., 2008; Tcharkhtchi et al., 2021).
There is still need to do a longer duration studies as well as the involvement of larger number of willing subjects because so far, most of the research report documentation on the time range for which patients wore the mask were within 45minutes to 12hours, (Roberge, et al., 2010; Scheid et al., 2020;) and case in point, the report of Roberge et al., 2010). This is not enough to make a justifiable conclusion that prolonged use of face mask has not clinically significant effect on the human physiological system, especially on respiratory parameters and body signs.
Judging and drawing argument on the fact that the reports did not state the compliance of the subjects used for the study and considering the number of subjects used for the study. No record was given to show that the subjects were continually monitored to ensure compliance. As of writing this review, only few detailed research has been carried out to study and evaluate the impact of prolonged used of face mask on health and this was cited in the report of Kisielinsk, (2021).
Since the study was basically for a short period of time that didn’t exceed a day period, the question that needs to be addressed is the effect of this face mask when for a prolonged period of time even exceeding a day.
They may not have an imminent effect but on prolonged period of time, they may cause health issues. Some other grey areas that needs to be addressed is that, were the pore sizes of the face masked examined to ensure that they conform to standard. If they did conform to standard, then there is need for them to be reported as this will help solidify their claims.
Other issue that was not addressed is the aspect and possibility of CO2 retention within the lungs. Elevated level of CO2 beyond normal range can be detrimental to health and its well known to be associated with respiratory and metabolic acidosis.
According the report of Kisielinsk, (2021), 44 scientific papers have been published showing the negative effects of wearing face mask and out these papers, only 22 of them were published in 2020 while the remaining half were before the pandemic. There report further revealed that that prolonged use of face mask has statistically significant effect on the patients and caused elevated level of carbon dioxide in the subjects.
The above finding further support the assertion that there is less scientific research on the effects of prolonged wearing of face mask and thus the need for critical review and more in-depth findings on the subject matter. More research needs to be done to monitor the likely effects of this face mask while wearing them on a longer period ranging from 24 hours to days as well as monitoring the likely effects during continuous activity for longer days.
Symptoms health issues as a consequence of human actions usually manifest immediately but over time, they begin to show. Even drugs produced pass through all the four stages of clinical trials and still at the 4th stage, they are continuously monitored to ensure no future effects.
The need for investigational study of the effects of face mask use on African populace
In April 2020, when the World Health organization generally recommended the use of face mask for health care providers, the essence was to ensure their safety and health but in June, 2020, they made an amendment to this by recommending face mask general use by the masses. This recommendation did not only encourage the use of face mask, it also contributed to the surge in price.
In addition, the recommendation failed to take into consideration some patients that might have underlying health conditions like breathing difficulty. It led to a lot of controversy and people who were not really accustomed to the use of face mask had to put them on regardless of what condition or health challenges they are undergoing.
Overtime, there has been a lot of concerns as reports of discomforts and side effects sprung out over time. On the long run, some people began to have the wrong notion that face shield can be used in place of face mask especially for individuals that may have breathing difficulties meanwhile in the real sense of it, face shield is meant primarily to protect the eyes from splash of body fluids from another person and it also meant to be worn in conjunction with face mask (Scheid et al., 2020).
Even though the importance of wearing face mask cannot be over emphasized, the need to also take into consideration its potential health effects when it is worn for a prolonged period of time is of paramount importance. As stated by WHO, (2020) in her documents explaining the guideline for the use of face mask, not all individuals need to wear face
mask.
Those who are not exposed to patients or have any contacts with patients need not wear the face mask unless otherwise. So far, there has not been any report or findings regarding the effects of face mask on African populace and this is really an issue worth addressing, possibly requiring more research.
Majority of the research done were not in Africa and considering the fact that environmental factors have huge impact on the efficiency and effectiveness of the face mask (Tcharkhtchi et al., 2021) and also the use of face mask is very important in curbing and reducing the spread of infectious diseases, the urgent need to delve deep into this area is crucial.
It is a well-known fact that Africa at large is a tropical region and as such, one would definitely expect and alteration in the properties of the
components used in the production of the face mask due to the hot temperature. This would require more research on for validation. As much as some of the face mask used in Africa case in point, Nigeria, are produced indigenously while some are imported, their properties and filtration efficiency are likely to differ because of the different environmental condition.
In the facility where I work, we have had cases of reinfection of corona virus among other health workers even though they wore the face mask consistently and have been following the guideline and protocols for prevention of covid-19. One would wonder, why are they still infected with
corona virus infection.
The answer to the question is not far-fetched, it could be due to some errors on the part of the individual but it is also very important to look at the efficiency of the face mask they wore. Has the face mask lost its particle filtration efficiency due to storage, use and exposure to the harsh weather conditions? Or was it an error on the part of the individual? There is also need to look at the material used in the production of the face mask.
Consumables and Products manufactured different regions are usually subject to different environmental conditions and most times slightly differ in performance and efficiency (Tcharkhtchi et al., 2021). Since the materials used in producing them are not exposed to the same environmental condition when worn, this therefore calls for a need to do an evaluation study and possibly compare the efficacy of these masks to affirm and confirm if they are actually effective as claimed by the manufacturers. When this is done, it will give more confidence and credibility to the claims made by some health institutions about the particle filtration efficiencies of these face masks.
The need for indebt research is of necessity and should not be overlooked.
Other reported effects
Reports have shown that the use of face mask cause other side effects such as headaches, rashes, contact dermatitis, urticarial, skin damage etc.(Foo et al., 2006; Ong, et al., 2020; Lan et al., 2021).
Some chemicals like Thiuram, which is found in the ear loop of the surgical mask and formaldehyde, which are some of the components of face mask have been reported to cause allergic reactions and some skin reactions in some individuals who use the face mask. (Badri, 2017).
Among the side effects associated with the use of face mask, the most prevalent and well reported is the skin reaction and headaches. One of the sub type of headache associated with prolonged use of face mask is referred to as cervicogenic headache and they are cause by the compression of the superficial nerves around the neck region. The pain is felt in the head but they originate from the neck and it has also been observed that for shorter duration, the headache is seeming to be less felt (Lim, et al., 2013).
Does benefit outweigh the risk?
No doubt, it is of fact that wearing the face mask offers some level of protection against infectious diseases like the SARS (Severe acute respiratory syndrome). The major aim of health care providers and health organization is to save life and not to add more problems. Now in a situation where the health of the patient is in jeopardy, the goal will ultimately be to save the life of the patient.
Wearing of face mask should be optional especially for patients that might have underlying disease and difficulty in breathing. Awareness campaigns is also of necessity to sensitize people on the proper use of this face mask.
Addressing surgical face mask use and the myths surrounding it
Since the emergence of covid-19, there has been series of different false assumptions especially in the developing nations. In the prevention of covid-19, regular washing, disinfection of the hands in addition to wearing the face mask properly is one key area in ensuring that there is less infection even though the use of face mask does not totally guarantee prevention of infection by the respiratory virus-covid-19.
The need for proper orientation on how to properly wear the surgical face mask has often been publicized in different media by health authorities like WHO. But still, there are some grey areas yet to be addressed critically.
The question remains this: how do you wear the surgical face mask. The question above cannot be answered without a critical study of the components, structure and main parts of the surgical mask.
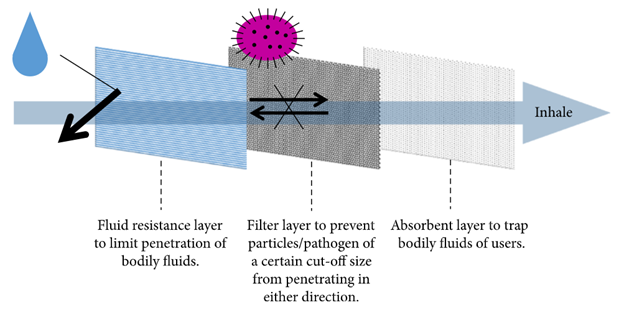
A standard surgical mask is made up of three layers (WHO, 2020).
The outer-hydrophobic layer (usually coloured): This layer by virtue of being hydrophobic repels fluids and contaminants from splashes emanating from others that might be carriers of respiratory disease like covid-19 as they talk, cough or sneezes (Tcharkhtchi et al., 2021).
The middle-filter layer: It basically traps germs and filter infectious agents while,
The inner moisture absorbent layer: Absorbs moisture when the wearer talks, speaks, cough or sneezes.
In essence, the face mask is designed as a one-way use personal protective equipment.
The myth: You wear the face mask with respect to your infection status. If you are infected, you are expected to wear the face mask with the in the actual right way and which is, the outer hydrophobic layer or coloured
layer facing outwards while the inner layer facing inwards. But if are not infected, you are erroneously expected to put on the face mask with the outer layer facing inwards while the inner layer faces outwards.
Face mask structure by Chua et al., CC BY-SA
The latter has actually been erroneously practiced even among health care professionals for some time now and there is need to address this before it causes more damage.
The fact: The only standard way to put on the face mask is with the coloured part facing outward while the inner part facing inward (WHO, 2020; Tcharkhtchi et al., 2021).
Putting on the face mask to prevent infection from infectious agents in the reverse direction will be doing the right thing the wrong way. The outer layer has been designed to repel fluids by virtue of this, if it placed to face the mouth of the wearer, fluids and moisture emanating from
the individual’s mouth will not be absorbed, thus resulting to quick accumulation of moisture around the mouth and the perinasal region (Guo et al., 2008).
Conclusion
As much as face mask play a huge role in the prevention of infections against respiratory diseases, the need to address the likely health implications, correct errors and false assumptions and myths surrounding its general use is very much important. There is need for further study as to really and without any shadow doubts ascertain that the general use of mask be it surgical or respirators does not pose serious health problem and challenges in future as a consequence of its use.
Aside the discomforts it has been proven to be associated with, it should be proven not to be associated with any serious potential health problem. People with pre-existing respiratory problem will find it difficult using the face mask appropriately and as such, cannot be forced to use it.
Breathing naturally is far better than breathing through obstruction.
Face mask use should be a last resort and not made as part of life style. Wearing this personal protective equipment may not cause any clinical significant alterations as seen in the literatures cited, but there are always long term pathological consequences of this at the long run. Hence, the need for proper campaigns and awareness about the future consequences of face mask prolonged consistent use is very important.
More research is encouraged in this regard to forestall any future health implications continuous and prolonged use of face mask might cause.
until I come your way again, bye for now.
References
- Badri FM. Surgical mask contact dermatitis and epidemiology of contact dermatitis in healthcare workers. Current Allergy & Clinical
Immunology, 2017, 30(3). - Chua MH, Cheng W, Goh SS, Kong J, Li B, Lim JYC et al. Face Masks in the New COVID-19 Normal: Materials, Testing and Perspectives, Research. 2020, 40. Article ID 7286735,
https://doi.org/10.34133/2020/7286735 - Cummins EP, Strowitzki MJ, Taylor CT. Mechanisms and
Consequences of Oxygen and Carbon Dioxide Sensing in Mammals. Physiological reviews. 2020; 100(1):463-488.
https://doi.org/10.1152/physrev.00003.2019. - Desai SR, Kovarik C, Brod B, James W, Fitzgerald ME, Preston A et al. COVID-19 and personal protective equipment: Treatment and prevention of skin conditions related to the occupational use of personal protective equipment. Journal of the American Academy of Dermatology. 2020; 83(2):675-677.
https://doi.org/10.1016/j.jaad.2020.05.032 - Foo CC, Goon AT, Leow YH, Goh CL. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome-a descriptive study in Singapore. Contact dermatitis. 2006; 55(5):291-294. https://doi.org/10.1111/j.1600-0536.2006.00953.x
- Guo YP, Li Y, Tokura H, Wong TKS, Chung JWY, Gohel MDI. Evaluation on Masks with Exhaust Valves and with Exhaust Holes from Physiological and Subjective Responses. Journal of Physiological Anthropology. 2008; 27:93-102.
- https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/clothface-cover-guidance.html#mask-adaptations-alternatives. accessed 25 may, 2021, 4:38am.
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks. Accessed May, 2021. 10:14pm.
- Kao T, Huang K, Huang Y, Tsai T, Hsieh B, Wu M. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. Journal of the Formosan Medical Association. 2004; 103(8):624-8.
- Kisielinski K, Giboni P, Prescher A, Klosterhalfen B, Graessel D, Funken S et al. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health. 2021; 18(8):43-44. MDPI AG. Retrieved from http://dx.doi.org/10.3390/ijerph18084344.
- Köseoğlu Toksoy C, Demirbaş H, Bozkurt E, Acar H, Türk Börü Ü. Headache related to mask use of healthcare workers in COVID-19 pandemic. The Korean journal of pain. 2021; 34(2):241-245.
https://doi.org/10.3344/kjp.2021.34.2.241 - Lan J, Song Z, Miao X, Li H, Li Y, Dong L et al. Skin damage among health care workers managing coronavirus disease-2019. Journal of the American Academy of Dermatology. 2020; 82(5):1215-1216.
https://doi.org/10.1016/j.jaad.2020.03.014 - Lim EC. Seet RC, Lee KH, Wilder-Smith EP, Chuah BY, Ong BK. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurologica Scandinavica. 2006; 113(3):199-202.
https://doi.org/10.1111/j.1600-0404.2005.00560.x. - Ong J, Bharatendu C, Goh Y, Tang J, Sooi K, Tan YL et al. Headaches
Associated with Personal Protective Equipment-A Cross-Sectional
Study Among Frontline Healthcare Workers During COVID- - Headache. 2020; 60(5):864-877. https://doi.org/10.1111/head.13811.
- Purushothaman PK, Priyangha E, Vaidhyswaran R. Effects of Prolonged Use of Facemask on Healthcare Workers in Tertiary Care Hospital During COVID-19 Pandemic. Indian J Otolaryngol Head Neck Surg. 2021; 73:59-65. https://doi.org/10.1007/s12070-020-02124-0.
- Rebmann T, Carrico R, Wang J. Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. American journal of infection control. 2013; 41(12):1218-1223. https://doi.org/10.1016/j.ajic.2013.02.017.
- Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ.
Physiological Impact of the N95 Filtering Facepiece Respirator on Healthcare Workers. Respiratory care, 2010, 55(5).20. - Rosner E. Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. J Infect Dis Epidemiol. 2020; 6:130. Doi. org/10.23937/2474-3658/1510130
- Scheid JL, Lupien SP, Ford GS, West SL. Commentary: Physiological and Psychological Impact of Face Mask usage during the COVID-19 Pandemic. International journal of Environmental. Research and Public Health. 2020; 17:66-55. Doi:10.3390/ijerph17186655.
- Shenal BV, Radonovich LJ, Jr. Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. Journal of occupational and environmental hygiene. 2012; 9(1):59-64.
https://doi.org/10.1080/15459624.2012.635133 - Smith JD, MacDougall CC, Jennie Johnstone, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. Canadian Medical Association Journal. 2016; 188(8):567-574.
https://doi.org/10.1503/cmaj.150835. - Strasser BJ, Schlich T. A history of the medical mask and the rise of throwaway culture. The Lancet, 2020, 396. (20) 31207-1.
https://doi.org/10.1016/S0140-6736 - Tcharkhtchi A, Abbasnezhad N, Seydani MZ, Zirak N, Farzaneh S, Shirinbayan M. An overview of filtration efficiency through the masks: Mechanisms of the aerosol’s penetration. Bioactive Materials. 2021; 6(1):106-122, https://doi.org/10.1016/j.bioactmat.2020.08.002.
- WHO Director-General's opening remarks at the media briefing on COVID-19. 11 March 2020.
- World Health Organization. WHO-Advice on the Use of Masks in the
Context of COVID-19: Interim Guidance, 5 June 2020; World Health
Organization: Geneva, Switzerland, 2020. Available online:
https://apps.who.int/iris/handle/10665/332293. Accessed may 2021.