In one of my previous post, we dwelt critically on the concept of apheresis and how this advanced method of blood donation has changed the landscape of medical practice and management of diseases, case in point, malignant cancers.

Image taken by @cyprianj
We were able to establish that for a fact, apheresis fills in the gap created by lack of specific blood components and products that may be specifically required by a sick patient.
One of the areas we forgot or will I say failed to address is the likely consequences of the procedure if it is not well performed. It us very important we address some of this effects because an error in the procedure can be fatal.
Apheresis procedure does not give room for incompetence. This post in essence is a sequel to the previous one and it primarily aims to answer some questions about apheresis besides explaining the likely consequences.
To read more about it, see it here - The era of personalized medicine and the role of blood components and products in blood transfusion medicine. Reading it will bring you up to speed on our discussion today. Let's get on with it shall we!
Should anything go wrong with apheresis procedure, what happens?
Judging from some of the components of the machine, one of the most delicate part watched out for is the Air bubbles detector whose function is to detect any air bubble that might be found inside the tubing of the machine. The big question you would want to ask is, what effect or danger does this air bubble have or why do we have to care about them?
When air bubbles find their way into the donor's blood system, they cause what is medically referred to as Air embolism (gas within the blood vessels of an individual). Air embolism does not only occur during apheresis, but also during administration of intravenous injections (IV).
Ever wondered why before that nurse injects you with drugs? One of the reason is to expel any air bubbles within the syringe. Another reason is to check and be sure that the needle nozzle or orifice is open.

Air bubbles while drawing IV injection
Air bubbles during apheresis usually occur as a result of ineffective suction pumps of the apheresis machine. These small pumps are basically responsible for pumping blood back to the donor's body after the required component of the blood has been extracted. When any of the strategically placed pumps fail, they create room for air to penetrate the tube and subsequently mix with the blood flowing back to the donor.
What happens inside the donor's body system that makes the bubble fatal?
The human body system is made of circulatory system with arteries and veins that ensures that both oxygenated and deoxygenated blood are delivered to organs and lungs in the body respectively.
The vein is mainly responsible for transporting deoxygenated blood from various organs to the heart and finally to the lungs where they are oxygenated and subsequently delivered to the heart, which in turn pumps the rich oxygenated blood to the whole body in general so that tissues and organs can use for metabolic functions.
Understanding of the above process simply gives you an idea of likely access routes of the air bubbles in the individual. Don't worry if you are still confused. a quick peep into the design of the human cardiovascular system will help you understand better.
Lets briefly discuss how the blood flows in us. Its quite interesting and I have something interesting to tell you. I am sure to some extent, you never have probably heard about it.
The human Cardiovascular system
As I earlier explained, the human body has a fluidic system that is made up of blood which can be deoxygenated or oxygenated depending. The heart acting as pump helps in the circulation of the blood throughout the body.
As you breathe in oxygen, it mixes with deoxygenated blood (blood without oxygen) in the lungs to become oxygenated, this oxygenated blood is the sent from the lungs to the left side of the heart through the pulmonary vein.
The blood then enters the heart through the left atrium passes through the left ventricle into the aorta. The aorta then supplies the rest of the body blood. Some go to the brain while others go to various tissues and organs.
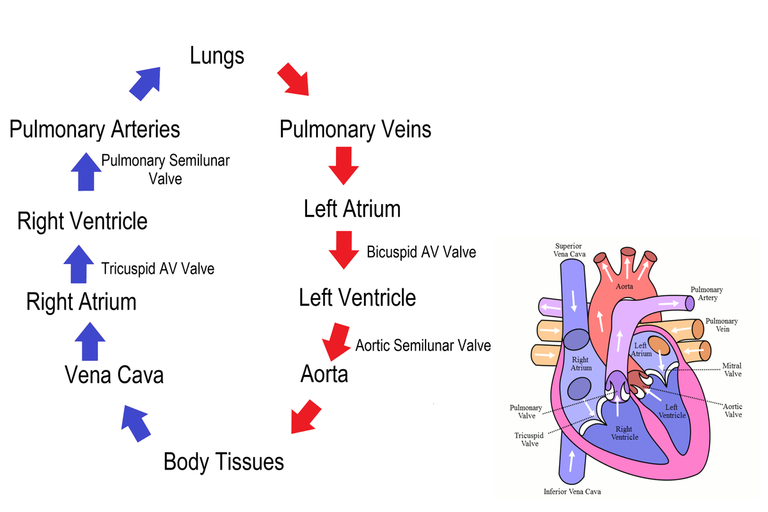
Circulation of blood through the heart
As the oxygenated blood enter tissues, carrying oxygen along, these oxygen is used up for metabolic processes that later yield various metabolic waste and one of which is carbon dioxide.
Since the blood has been sapped off its oxygen, it becomes deoxygenated and thus return from the tissues with its carbon dioxide content through the veins straight to the heart.
Through the Vena Cava, the deoxygenated blood enters the heart passing through the right atrium and the right ventricle where it is passed to the pulmonary arteries and straight into the lungs where is oxygenated once again.
The real gaseous exchange (addition of oxygen to the deoxygenated blood) through our breathing process, the oxygenated blood is again pumped backed to the whole body for usage. The cycle continues on and on till death.
Now, recall that the veins obviously returns blood back to the heart. When air is introduced into the donor through intravenous line (connection of fluid passed into the veins), because air is not soluble at that point, as we have seen from the circle earlier, the air will go straight to the heart and then to the lungs.
Inside the lungs, the air will cause most of the surrounding blood vessels to constrict (reduce or shrink in size) and this can even lead to lungs collapse and respiratory failure.
Further implication of this is that, it will raise the vascular pressure in the pulmonary veins. Remember that, the pulmonary vein carries oxygenated blood from the lungs to the heart from which it is pumped to the brain and other parts of the body.
This raised excessive vascular pressure in turn can even cause an increase in heart pressure and even further block coronary arteries of the heart thus, resulting to heart attack or even heart failure.
The most fatal case is when manages to get to the brain. As the air travels from the heart to the brain, it cause an occlusion of blood supply to certain areas of the brain and this subsequently leads to stroke.
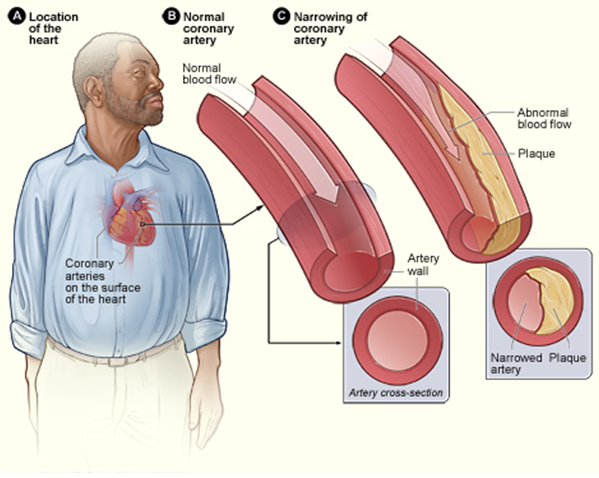
Narrowed coronary arteries causing heart attack and even stroke in humans
This can even be worst in people who already have pre-existing heart problem. Anything that occludes or prevents the free flow of blood in the heart can cause heart attack.
Some commercial blood donors (donors that willingly come to the hospital to donate blood in exchange for payment) lie a lot just for money and and approval to be eligible for blood donation or apheresis.
For no reason must you lie to the medical staff prior any medical procedure, patient history are very important before any procedure or treatment is carried out. Any wrong information supplied can be detrimental your your well being.
The above is one of the reason apheresis procedure if not well handled can prove fatal. Of utmost importance, quality checks is very essential before the machine is used on patients.
You might want to ask, the air bubble sensors, are they not there to detect the air bubbles and stop the machine? Your question is hundred percent valid, but remember, when they are not well calibrated, they tend to malfunction. So in essence, strict guidelines for servicing and maintenance of this machine is of utmost importance.
Now to what I promised to tell you earlier. For a fact the heart is generally located on the left side of the chest and it is protected by the rib cage. In normal heart, it is positioned in the left thoracic cavity and pointing left.
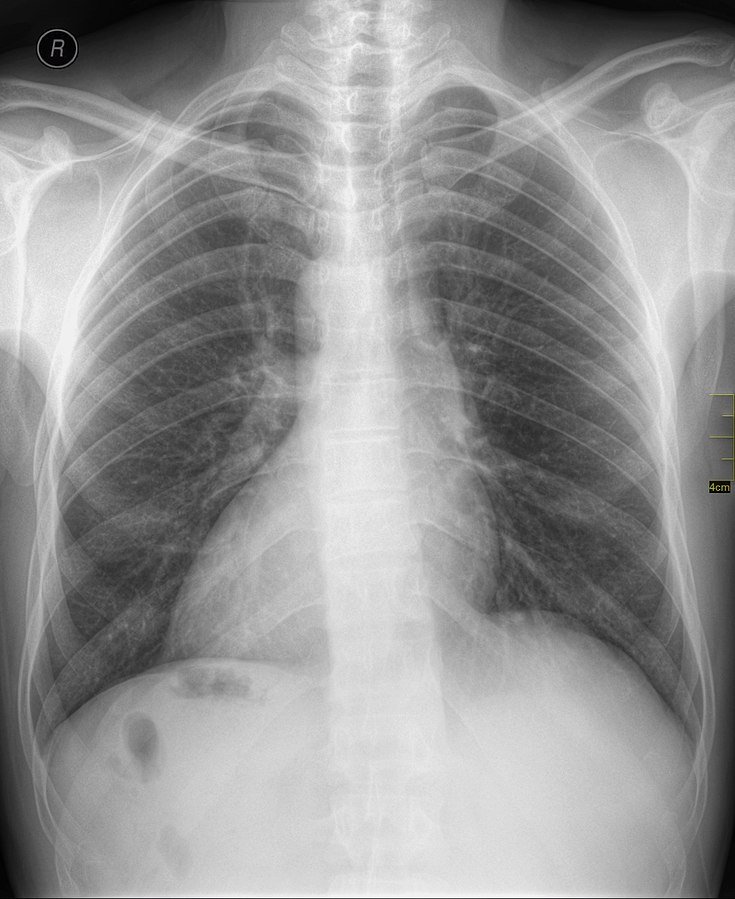
An X-ray showing a heart located on the right side, Situs inversus
What if I tell you that some people have their heart located in right side of their thoracic cavity. This abnormal condition is referred to as Cardiac Dextroposition.
Cardiac dextroposition is the horizontal displacement of the heart into the right hemi thorax. Dextrocardia, on the other hand is a condition where the cardiac apex is displaced to the right side due to a rotation on its own axis. Dextrocardia can be associated with inversion of other internal organs called “situs inversus"
When it is a condition causing a change in the position of the apex of the heart, it is generally also referred to as Dextrocardiac. So it is not everyone that has their heart located on the left side, some may have theirs on the right.
Secondly, note that if someone (a normal person with heart on the left) is stabbed with similar force to both side of the chest, the depth of penetration will be less on the left side than on the right side reason being that, the left side of chest that houses the heart is naturally more thicker than the right.
This is just a natural protection since the area houses one of the most important structure in humans. I am sure you have learnt some possibly new.
Other likely fatal consequences of Apheresis
Besides the presence of air bubbles within the circulatory system of the donor, another likely consequences of apheresis is the Haemolysis of blood cells. Haemolysis simply means the lysis or bursting of the red blood cells, resulting to the release of the intracellular contents the blood cells.
The contents of the blood cells are toxic and as such cause severe acute reaction within the donor. This reaction is similar to that that occurs during transfusion due to blood group incompatibility. These reaction trigger severe fever (critical rise in the body temperature greater than 42 degree Celsius) in the donor body system.
Haemolysis occurs mostly due to a wrong procedural method applied while handling the machine (one of the reason, a well trained personnel is only allowed to operate it).
Donor red cells may be damaged during apheresis procedures, releasing haemoglobin. Equipment malfunctioning valves, kinks or obstruction of tubing, incorrect installation of equipment, or other equipment failures affecting the extracorporeal circuit, most commonly cause this. In addition, incompatible replacement fluids, such as dextrose D5W, may be used in error.
Sometimes the fluids used to replace the extracellular fluid imbalance caused by the procedure may not be well tolerated by the donor's body system and thus, this can result to haemolysis of the patient's blood.
Most of these reactions are intravascular haemolysis (occurs within the donor's blood vessels and thus can be more dangerous since they can get to the brain to trigger the temperature center in the hypothalamus of the brain).
Another area of concern is the tendency of the anticoagulant used for procedure, accidentally mixing with the physiological saline or the replacement fluid. Trisodium citrate is the major anticoagulant used for coagulation procedures and this chemical helps in chelating (removing) calcium ions that are required to initiate blood clotting process.
As they remove calcium from various tissues and cells, the most tissue that will suffer the effect is muscles and neuromuscular tissues because calcium plays a huge role in the release of important chemicals like acetylcholine needed for neuro transmission of impulses, reflex and signals.
In fact, without calcium, insulin cannot be released to mop up excess glucose from the body circulation and as a result, this can lead to diabetes. The role of calcium in the body is limitless.
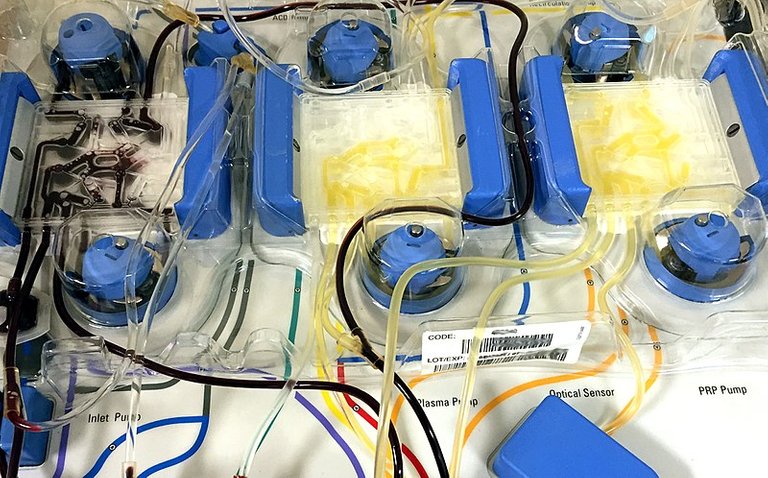
Confusing apheresis tubing arrangement
Since there is less calcium as against the concentration needed to initiate some actions in the body like contraction of muscles of the heart, hands etc, these functions are automatically halted and if care is not taken, it can cause tetany (continuous generalized involuntary muscle contraction).
The other effects of calcium are just too numerous to be discussed here. Mere looking at the arrangement of the tube above in he image above will give you an idea of how complex it can be. If one is not well trained, the tendency to mix the tubes are there and this can result to wrong infusion of the anticoagulant.
You might want to ask, but why then is anticoagulant in the procedure. The answer is pretty simple, remember that the blood as it exits the human body systems where it also has natural anticoagulant that keeps it not coagulated (form clumps), the blood is bound to clot.
Anticoagulant prevent blood from clotting. As the blood gushes out of the donor through the IV line, it mixes directly with the anticoagulant to prevent clotting within the tubes of the apheresis machine.
If by any chance, the blood clots, it can block the tubes of the apheresis bag and this can lead to wastage. Just to burst your bubble, in my facility, a single apheresis bag cost as much as $300 and when service charges are added, the total fee usually paid can be as high as $400.
As a donor, the moment you start feeling some of these symptoms such as dizziness, nausea or maybe as a medical staff, you observe a low blood pressure in the donor, it is better to stop and check the aetiology (origin) before continuing with the procedure.
Can one donate through apheresis as often as possible? Well, it depends of what is being donated. If it is plasma, yes you can. Plasma can be easily replaced since its major content is water. When you are adequately hydrated, plasma donation can be done even twice a week.
This cannot be done for platelets because it has huge role to play in the body and moreover, there is a particular concentration you must have before you are fit for donation of platelets. The risk of internal bleeding to death is associated with severely reduced platelet level.
In conclusion, apheresis even though an awesome technique for management of some disease conditions, it could also pose potential threat to life if not well carried out. Though some of the listed consequences doesn't happen all the time because of the extra measures that have been put in place to ensure that the machine, tubes, valves, pumps, optical sensors etc are functioning optimally.
An advantageous procedure can become a disadvantage if not well executed and handled by the best hands and with extra caution.
Until I come your way again, stay awesome.
References
•Complications of transfusion
•Adverse events in apheresis: An update of the WAA registry data
•Adverse events associated with apheresis procedures: Incidence and relative frequency
•Dextrocardia
•A heart on the right can be more complex than it first appears
•An unusual cause of acquired cardiac dextroposition
•Complications related to apheresis
•Adverse events associated with apheresis procedures: Incidence and relative frequency