The motivation to write this article came from one very important question I was asked by @gentleshaid in the comments section of my previous post. This will likely be a short or a long read depending on how far I am able to bring the point home through in-depth and easy to understand explanation. It will be more like an extension of the previous one to further explain some things that really need more elaboration.
Reading this article will give you a full picture of what really happens in the clinical settings. Sometimes, the theories you are taught in school may not always play out well in practice, they may sure be the foundation, but alot of modifications always come into play when need be. In any case, sit tight and enjoy.
Agglutination reactions caused by cold agglutinins
To help understand what I will discuss in this article, you can always make reference to this article I wrote about two months ago - Blood group O is not a universal Donor; why?. This article will bring you up to speed definitely and some of the questions you might want to ask would have already been answered in it. However, there is usually a weird thing that happens during cross matching of blood between the donor and the recipient serum.
Just to remind us that, reacting similar blood with another corresponding blood group in ideal situations are not meant to react and cause agglutination because they do not have any antibodies against each other. I.e blood group A and another blood group A cannot react to cause agglutination since they are the same and contain the same antibodies that are not against each other.
Shockingly, through experience in the clinical practice, it has been observed that there are times when compatible blood groups still cause reactions in the recipient. This case is usually detected during cross-matching process prior blood transfusion. A donor's blood may be by theory compatible, but in reality, it is not due to what is known as agglutinins. When you hear of cross-matching, always remember that it simply means mixing the blood of the donor with the serum of the recipient.
In clinical practice, cross matching is done (invitro) to show how the blood will be accepted invivo (inside the body of the patient). It is just like seeing what will happen inside the body in a test tube. If the blood react inside the test tube, then it will sure react Inside the body of the patient. Whatever that will happen to the patient is seen easily in the test tube. It is a very sensitive process that is never rushed for any reason.
If you would recall, we discussed in details why blood group O+ cannot he referred to as a universal donor because of the presence of haemolysin that can be present in some of them and in high titre, they cause transfusion reactions. There are conditions that can also cause your body to react especially during cold conditions. Cold Agglutinins happens to be another issue that is usually tackled before a blood is considered safe for transfusion.
Blood film showing red blood cell agglutination due to cold agglutinin
In the image directly above, the round cells with central parlor are the red blood cells while the larger one at the center with 4 blue-purple coloured nucleus is the neutrophil. The larger clumps of red blood cells is the agglutination caused by cold agglutinins. This is mainly clearly visible in this case only with the use of a microscope set at ×100 objective lens (aka oil immersion lens).
It is funny when patients pressurized medical personnels regarding investigation results. The truth is that, a lot of things go on behind the scene and one of which is the complexities associated with blood transfusion. If anything goes wrong, the consequences are usually fatal, especially in cases of severe reactions in post transfusion.
How cold agglutinin came about?
Cold Agglutinins are autoantibodies (against self), that are produced by the body against red blood cells. It is rare but very much in existence. They cause a type of of anaemia called autoimmune haemolytic anaemia. They are mostly activated at lower temperatures. Specifically, they are more active at ideal refrigeration temperature of less than 4 degrees Celsius. For this reason, they are referred to as cold agglutinins. The problem with cold agglutinins is usually encountered mostly using a blood that has been kept in the blood bank refrigerator.
No doubt, the essence of keeping donated blood in the blood bank refrigerator, is to preserve the blood for the patient pending when it will be needed, mostly in cases of surgery, child delivery and in emergency situations. During the period of storage, the blood gets cold and in the process of transfusion into a patient who has the cold agglutinin disease, it reacts and cause agglutination.
Cold agglutinins are normally made by the immune system in response to infection. They cause red blood cells to clump together (agglutinate) at low temperatures.
Healthy people generally have low levels of cold agglutinins in their blood. But lymphoma or some infections, such as mycoplasma pneumonia, can cause the level of cold agglutinins to rise.
People with cold agglutinin disease are never given blood from the blood bank refrigerator, rather, they require refresh donated blood that must not in any way be kept in the fridge. The presence of Cold agglutinin doesn't care about the blood compatibility, whether the blood is compatible or not, so far the blood is cold, it will react in the patient.
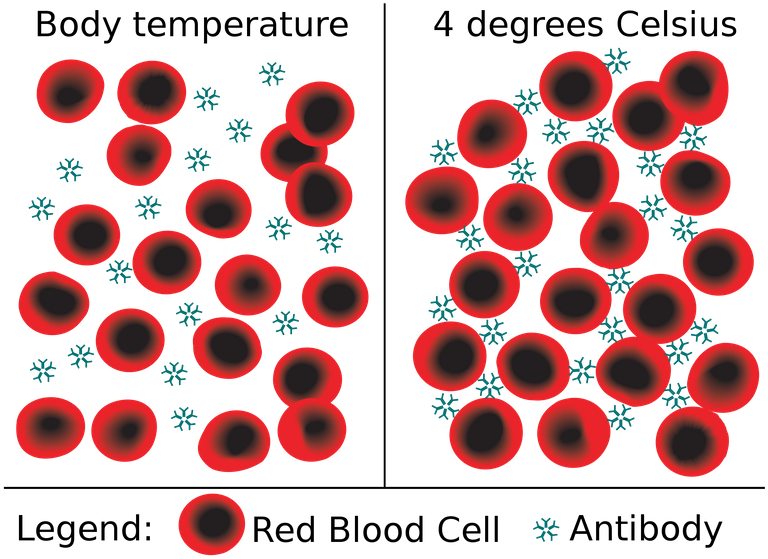
Agglutination reactions caused by cold agglutinins
This is one of the reasons, cross-matching is done. If you don't do cross-matching and just go ahead to transfuse a patient, if the individual has the disease, the consequences will not be funny. In most cases, cold agglutinin reactions causes destruction of the red blood cells and this lead to anamia (low blood volume). Individuals with cold agglutinins usually react when their body is exposed to cold temperatures.
Having explained the above, it is pertinent to emphatically say this; a blood might pass compatibility testing involving ABO blood groups and Rhesus system, failure to pass the cross-matching test and also the agglutinin test if suspected means that the blood cannot be given to the patient. In essence, blood group compatibility is not the only criteria for a safe transfusion.
People with cold agglutinin disease, besides reacting during cross matching or during transfusion, they can also react when they are in cold environments that cause their body temperature to drop. They usually experience frostbites and this reaction happens at the extremeties of the body,m which are obviously less hot.
The reaction can subside if they find themselves in warmer environment. In severe cases, the condition can to lead gangrene (death of tissue caused by lack of blood flow to the area in question).
One of the easy way to confirm if a patient has cold agglutinin, is to prepare a thin film section of the patient's blood. The procedure is simple and requires you, placing a drop of blood 3/4 on a glass slide and with a spreader, you spread the blood on the glass slide. Upon macroscopic examination of the dried blood film, you would notice the some changes in the blood film when you placed in different condition of temperature - cold and warm (37 degrees Celsius)
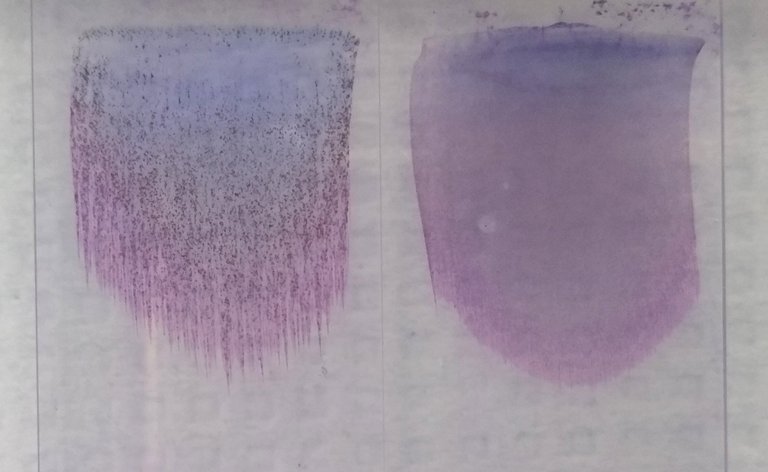
Observable macroscopic changes in blood smear of a cold agglutinin disease patient
Two stained blood smears from a patient with cold agglutinin disease. The first smear (left) was made while the sample was at room temperature: the red blood cells are strongly agglutinated, causing the smear to appear grainy. The second blood smear (right) was made after incubating the sample at 37 C, which weakens the agglutination.
Other situations that can lead to post transfusion reactions
Besides the ABO blood group incompatibility, presence of haemolysin, Rhesus incompatibility, and cold Agglutinins, multiple blood transfusion of a patient involving different blood group can also cause post transfusion reactions in a patient. Let's explain this better.
Case scenario involving Mr. Fortune
Mr. Fortune is a patient who has been diagnosed of chronic cancer - lymphoma and as such will require blood transfusion. From laboratory investigation, he was confirmed to be of blood group A rhesus D positive (A+) - meaning he can only receive blood from a group O+, O-, A+ and A-. From his medical history, he has had over 9 blood transfusions in the past and the record also shows that all the blood transfused were all from blood group A+ blood of different donors.
In clinical practice, since Mr. Fortune has been receiving blood group A+, it is wiser to continue with blood group A+ because there is a chance that he might have acquired some other types of antibodies from the various A+ blood group donors. Recall that you develop or produce antibodies against any blood group you do not have.
In essence, the chances are always high that Mr. Fortune might have been sensitized by other types of antigens leading to the production of other types of antibodies, though present but won't cause any obvious harm unless another type of blood is given to him.
Just for the record, ABO and Rhesus blood group are not the only blood group system in existence. The ABO and Rhesus system are more discussed because they pose significant danger and threat to human life during blood group compatibility testing.
As of June 2021, information from the International Society of Blood Transfusion (ISBT) reveals that there are a total of 43 blood group system. Besides the ABO and Rh blood groups we already know, there are other types like the Kell, Duffy, MNS, Lutheran, Lewis, Kid, Diego, Yt, XG, Dombrock, Landsteiner Weiner, Chigo etc. These one are not much of important as compared to ABO and Rh. I guess you probably didn't know this until now. Congratulations, you just got more knowledgeable right now.
Regarding Mr. Fortune case, the best thing to do is to continue with giving him blood group A+ or A- provided it is available, if not then blood group O- should the be the first point of call before giving O+ which is much more readily available than blood group O-.
However, bear in mind, besides cross matching, haemolysin test must be done to ensure that the O+ blood doesn't have any form of haemolysin which has the ability of lysing or destroying the red blood cells of the patient or recipient. Remember we have been able to discuss and understand that blood group O+ is not a universal donor rather it is O-, you can read more on this in the earlier post I share at the beginning of this article.
Common practice to play safe and prevent post transfusion reactions
Depending on the state or condition of the patient, those that are healthy can donate their blood prior any surgery or any medical procedure that will require blood and later the blood is still transfused back to them afterwards. This act of donating blood is what is referred to autologous blood donation.
This is the safest form of blood donation because, it won't require all the screening and cross matching processes and in addition, there is zero chance of post transfusion reactions since it is still your blood that is being transfused back into you.
Autologous blood donation is also needed in cases a patient is known to react often to most other blood groups. So best thing to do is to bleed the patient prior surgery or any invasive procedure that could likely lead to extreme loss of blood.
In addition to the above, freshly donated blood is more healthier than blood that has been kept in the blood bank refrigerator for longer time. Not all blood components are stable in the refrigerator, e.g platelets (plays role in blood clotting). Donated blood in blood bank have a maximum life span of 35days. In specific, red blood cells can survive for that long but not platelets. This is why old blood in the blood bank is given more to anaemic patients while freshly donated ones are given to patients that are actively bleeding since the platelets will help arrest the bleeding.
Active bleeding is associated more with women who had just given birth, had miscarriage, had abortion or ectopic pregnancy. If the bleeding is not arrested early enough, it poses grave consequences and one which is bleeding to death. Really, you wouldn't want to experience complications in birth, it can be traumatizing.
Remember, you are welcomed to donate, to save lives. Donating blood helps both you and the patient because, you are saving a life and at the same time improving your health. When you donate blood, you tend to loose some cholesterol, and other likely substances that can pose a threat to your health once they are in excess. By donating blood, you authomatically reduce their concentration.
When you donate blood, you authomatically allow the bone marrow to produce more healthy red blood cells to replace the ones you lost.
I conclude here by saying that blood group compatibility is not enough criteria to confirm a blood safe for transfusion, antibody screening through cross-matching must be done as well as agglutinin test once it is suspected a patient reacts to blood group O. It is the easiest way to find out about those with cold agglutinin disease. Having the same blood group does not guarantee a safe transfusion without post transfusion reactions.
@gentleshaid has been set as 5% beneficiary of the reward from this post for instigating the write up through his question.
Until I come your way, stay awesome.
References
•Cold Agglutinins Test
•Cold Agglutinin; an overview
•Cold Agglutinin Disease Signs, Symptoms, Causes, Tests, and Natural Treatment
•Rare blood types
•Red Cell Immunogenetics and Blood Group Terminology
•Getting a Blood Transfusion