Transfusion medicine is vast and mainly revolves around all the possible situations that could arise while carrying out any form of transfusion in humans. Today's discussion will focus on a very important procedure that is a must-do for all pregnant and intending mothers. It is very crucial that determines a lot. The results from this test can guides prognostication.
A lot has been written about blood transfusion and fortunately, I have done my best to simplify blood transfusion medicine to even the layman. Reading some of these posts below will put you on the right track in understanding the fundamentals of blood transfusion medicine, and even advances therein.
•Blood group O is not a universal Donor; why?
•Is there a possibility of similar blood groups Cross-reacting to cause post transfusion reactions?
•Washing of red blood cells, a possibility or not; How and why?
Those posts are detailed enough to help you understand the basics of transfusion medicine. The test procedure we will focus on today is called the Coomb's test, which is further divided into Direct and Indirect Coomb's test. Let's briefly talk about them before going into their respective diagnostic procedures.
Schematic diagram of Coomb's test
Introduction
Before now, there were usually cases of transfusion reaction, stillbirth, miscarriages, etc. amongst pregnant women. The history of blood transfusion dates back to 1665 and to date, it has become a very useful practice that has saved a lot of lives, even though it has its other sides.
The consequences of mismatch in blood transfusion and compatibility testing are the major area of concern when it comes to diagnostic testing. The main aim of all compatibility testing is to ensure that the blood to be donated or transfused into a patient is safe and matches the blood of the patient.
Blood transfusion and its products are mainly necessitated when their level falls or when there is a medical condition that causes a decrease in the number of blood cells or their ineffectiveness in carrying out their physiologic functions. Some of these conditions can be severe and ultimately lead to fatality.
Some of these conditions include Rhesus haemolytic disease of the newborn, autoimmune haemolytic anaemia, and Drug-induced haemolytic anaemia (this is caused by drugs that can cause the body's immune system to attack and destroy its own cells). During blood compatibility testing, the major thing looked out for is the presence or absence of the antibody that could be responsible for the autoimmune reaction.
There are diagnostic that is a designed to detect the presence of these antibodies. This test is known as Coomb's test. Depending on the approach used, it could be a direct or indirect Coomb's test.
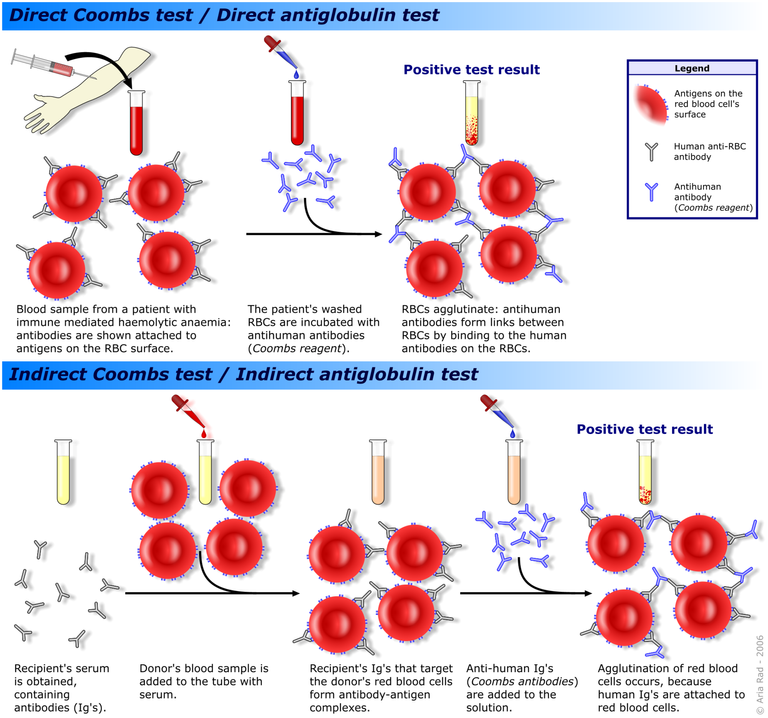
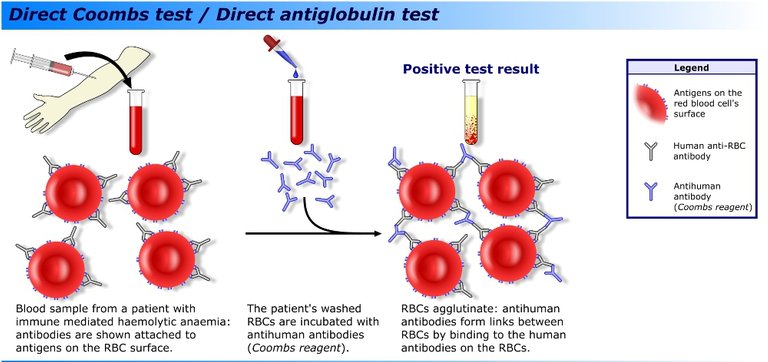
Antibodies produced in vivo in response to either drug-induced haemolytic anaemia or just immune-mediated haemolytic anaemia can be detected through the method known as Direct Coomb's test. Most of the antibodies produced against the body's cells are seen attached to the red blood cells' surface causing them to be destroyed.
Schematic of direct Coomb's test
They become attached to the surface antigen of red blood cells to cause haemolysis when they are induced by foreign blood antigens. In a nutshell, direct Coomb's test aims to detect those antibodies that are produced against the body's own cells.
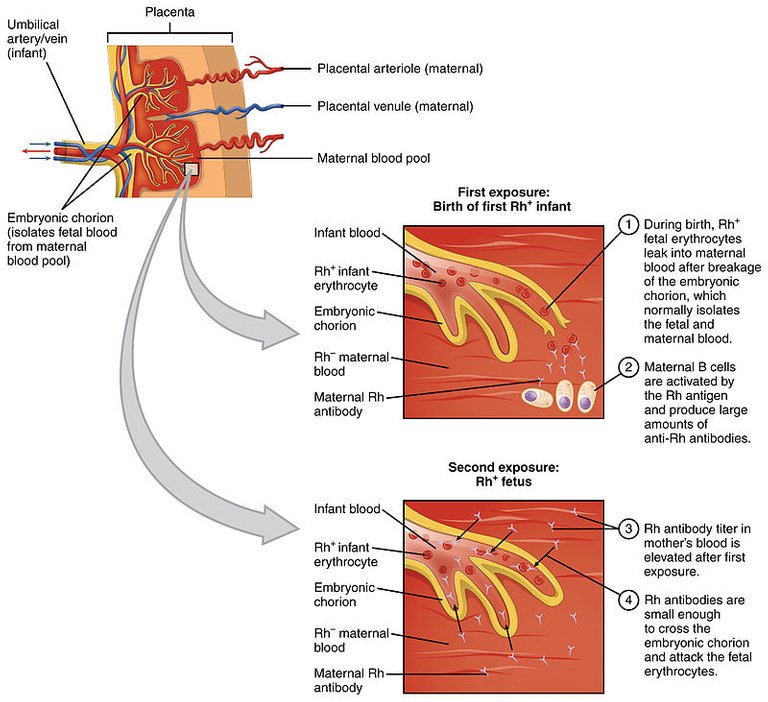
On the other hand, there are situations where due to Rhesus incompatibility, a pregnant mother may have been sensitized by an incompatible baby's blood during delivery. This mostly happens when a woman who is rhesus negative marries a man who is rhesus positive and gets pregnant with a rhesus positive baby. Because the woman does not have a rhesus antigen, her body system's immune cells recognize the blood of the baby as foreign and as such produce antibodies against the baby's blood.
To have a better understanding of Rhesus haemolytic disease of the newborn, you can read this post - detailed explanation on the challenges facing neonatal cross matching. You sure will gain a better understanding of Rhesus incompatibility. When the mother is sensitized, it simply means she has antibodies produced against the baby that are freely circulating in her serum. These antibodies if not detected within 72hours of delivery, can cause continuous death of babies subsequently. To avoid such issues, Indirect coombs testing is done.
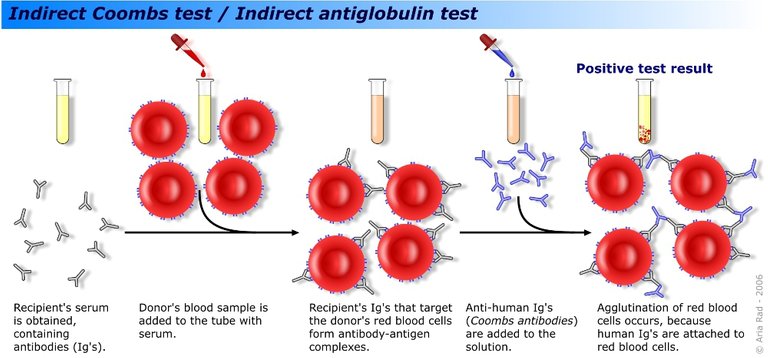
Schematic of indirect Coomb's test
Rhesus incompatibility is usually a case when the pregnant woman is Rhesus O negative (i.e. she has never been sensitized) and giving birth to a Rhesus positive child. The chances of the woman being sensitized by the Rhesus positive blood of the baby is high, hence, doing an indirect coombs test after birth will determine if the woman will be given Rhogam injection within 72hours of childbirth or not.
In patients suffering from drug-induced haemolytic anaemia, the major thing observed is the destruction of the blood cells by the antibodies that have been produced against the blood cells. The continuous destruction of the blood cells by the antibodies leads to anaemia (a decrease in haemoglobin concentration in the blood). Patients with anaemia end up requiring blood transfusion to ameliorate and counterbalance the lost blood.
In all, a positive direct Coomb's test simply means that an individual has an underlying condition that is causing blood cells destruction and means that the patient has antibodies attached to his or her red blood cells while positive indirect coomb's testing in pregnant women is an indication that they have been sensitized by the blood of their child and thus would require Rhogam injection to mop the antibodies before they are fully matured.
As a rule, indirect coombs testing is usually requested during antenatal testing to know the Rhesus status of the mother. A good understanding of the major stages of compatibility testing or cross-matching is very important to avoid cases of incompatibility reactions. Let's critically discuss the stages involved in this diagnostic procedure and then later we will discuss the stages of blood compatibility testing.
General principle of Coomb's agglutination reaction
To run a Coomb's test, you will in all cases need the Coomb's Reagent aka Antihuman globulin (AHG) reagent. This reagent is usually produced by injecting human globulin into a rat or an experimental animal. This animal's body system detects the human globulin protein as a foreign antigen, and in turn, produces polyclonal antibodies specific to the globulin.
You can read more about how monoclonal and polyclonal antibodies are made in these post - Latest groundbreaking findings from Cancer studies thus far; There is hope for our generation.
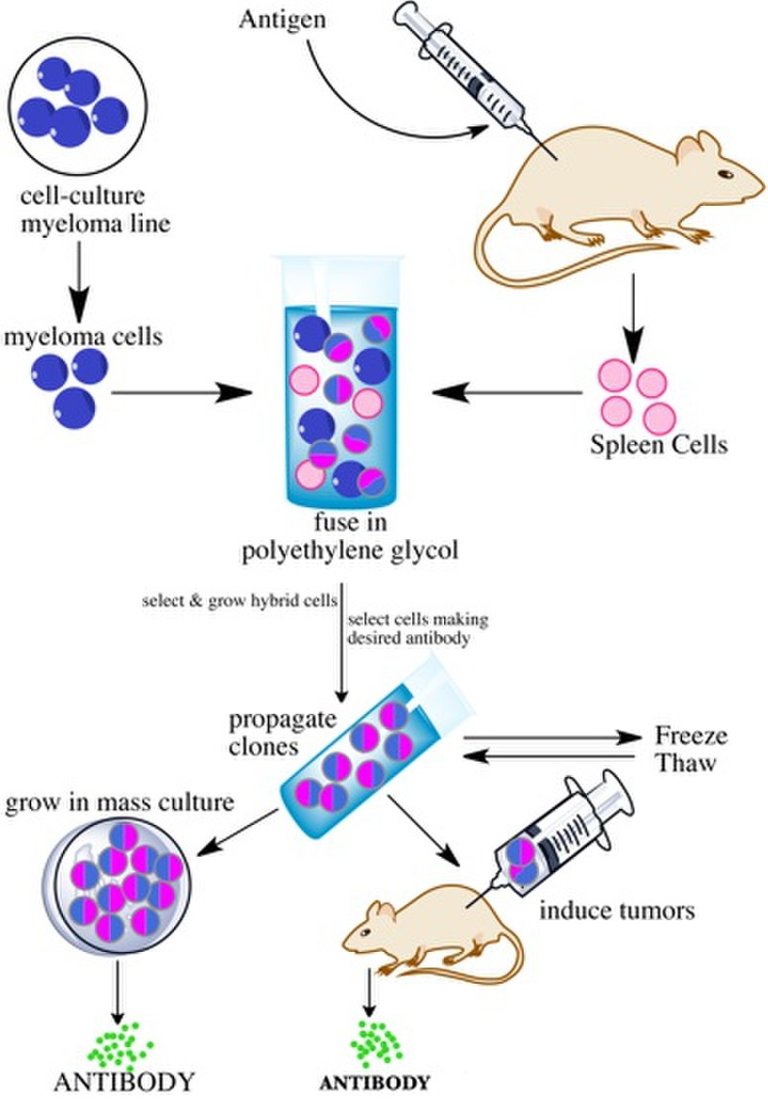
Monoclonal Antibody production
This reagent mainly is responsible for facilitating agglutination reaction between the antigen and antibody in already sensitized red blood cells. Sensitized red blood cells already have antibodies attached to their surfaces but these antibodies are not strong enough to cause an agglutination reaction or shrinking of the red cells.
The addition of Coomb's reagent enhances the reaction by acting as a bridge to link all the antibodies if present, thereby causing agglutination.
Direct Coomb's testing procedure
Recall we earlier explained the basis of direct Coomb's testing. It is very important to first wash the red blood cells and to do this, you need normal or physiologic saline. Washing the red blood cells helps to remove impurities, unveil the antigenic sites of the red blood cells, and also remove peptides that could neutralize the Coomb's reagent.
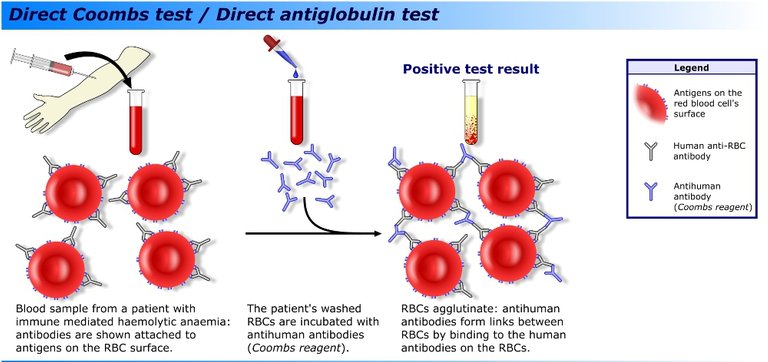
Schematic of direct Coomb's test
After washing the red blood cells, you then mix the blood directly with the Coomb's reagent. Since the antibodies produced as a result of autoimmune response, and are already attached to the antigens on the surface of the red blood cell, the addition of Coomb's reagent causes an agglutination reaction so long as the sample of the patient contains antibodies.
The presence or absence of these antibodies can be confirmed as a presence or absence of visible agglutination reaction which can be visualized physically under white light or using the microscope. The procedure is quite different in the case of indirect Coomb's testing.
Indirect Coomb's test procedure
There is a reason for the name indirect Coomb's test. In an indirect Coombs test, you do not directly add the antihuman globulin reagents to the blood of the patient, rather, the serum of the patient is obtained and mixed with a washed and pooled O rhesus D positive blood (pooled O+ cells are gotten by mixing different O positive blood, thereafter washing the using normal saline). The essence of this is to sensitize the blood.
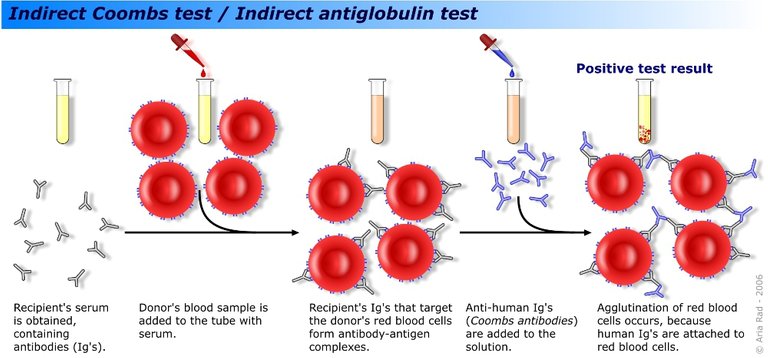
Schematic of indirect Coomb's test
If there are antibodies present in the serum, the blood will be sensitized (binding of the antibodies to the antigens on the surface of the blood) and this makes the blood susceptible to agglutination reaction. After the sensitization, the cells are washed again to remove excess and unbound antibodies, and subsequently, the AHG reagent is added to the mixture. Remember, the sole purpose of the AHG reagent is to make any sensitized cell reaction more visible in the form of an agglutination reaction.
All the reactions above occur better at the body's temperature, hence, for every step, with the exception of the washing stages, the mixture must be incubated at 37 degrees Celsius.
Indirect Coomb's test is a very important test that must be done on all intending pregnant mothers so as to know their status. If this test is not done and it happens that the woman is rhesus negative and with a rhesus positive child, the first child may survive but subsequent children may not and this will result in stillbirth (death of a baby before or during delivery) and miscarriages every time the woman takes in. This type of condition results to what is known as Erythroblastosis fetalis or Haemolytic disease of the newborn.
Early intervention with the RhoGam injection can save the woman from permanently developing Rhesus antibodies. It mainly mops up the antibodies and prevents the woman from developing any form of Rhesus antibodies in her system. For every delivery, she must be given the RhoGam injection within 72 hours.
Coomb's testing is indirectly incorporated into a very important stage of cross-matching. Let's quickly describe these indispensable steps and why they are very important in clinical practice.
The critical stages of cross-matching
Cross-matching is a test that must be done before any blood is given to a patient during transfusion, and it involves mixing the patient's serum with the donor's blood and then subjecting it to various conditions to see if there will be any form of reaction.
The presence of reaction simply means that the blood is not compatible and hence cannot be transfused to the patient. You can as well call it a major crossmatch. This test has majorly 3 stages commonly known as - the Normal saline stage (room temperature), Albumin stage and the AHG stage. We will look at them one after the other.
Normal saline stage
The normal saline stage or room temperature stage simply involves suspending the mixture of the patient serum and the donor's washed red blood cells inside a test tube and incubating them at room temperature. The major type of antibodies that is detected at this stage is the IgM antibody which mostly reacts at room temperature.
If it is present, there will be a visible agglutination reaction inside the tube, but if absent, no agglutination is seen. Next stage is the Albumin stage or the Thermo phase with a protein.
Albumin stage
This stage as the name implies, involves the addition of a protein such as bovine albumin into the mixture. The main function of this protein is that, it helps to breakdown the negative charges around the red blood cells so that they can come together to react as long as they are sensitized.
Bovine albumin facilitates the reaction and ensures that agglutination occurs in situation where the cells are already sensitized. After adding the bovine albumin, the mixture is then incubated for 30min. If the serum of the patient has antibodies, it will be seen as an agglutination reaction, hence, the blood is not compatible, but if otherwise, then it is compatible.
This stage mainly detects IgG antibodies that mostly react at body temperature of 37 Degrees Celcius, hence, the reason for the incubation st 37 Degrees. The last stage is the AHG stage, which can also be referred to as the Coomb's test. This is the stage we earlier talked about how Coomb's test is incorporated into cross matching.
The AHG stage
This stage is no different from the indirect Coomb's testing we earlier described above and the main aim is to also detect IgG antibodies.
If after passing through all the stages described above and there is no visible agglutination seen, then the blood is deemed fit for transfusion. On the average, the whole procedure should take not less than an hour. Because of the delay and long turn around time for this test, in cases of emergency, it is in most cases not done. Rather, an emergency Cross matching is done.
Emergency Cross matching simply involves directly mixing or reacting the serum of the patient with the blood of the donor on a tile or tube. Presence of agglutination is an indication of incompatibility while absence means that the blood is compatible.
Conclusively, cross matching plays a very important role in determining how safe a blood is. The ability to run this test accurately and give accurate results will determine if the patient will have a post blood transfusion reaction or not. Major cross matching is also a critical procedure prior transfusion. Coombs reagent is also the major reagent that facilitates the agglutination reaction in cases of weak sensitization.
References
•Coombs Test
•Coombs Test - Clevaland clinic
•Clinical applications of direct antiglobulin test
•Cross Matching for Blood Transfusion
•Bovine albumin function in blood cross-matching
•Cross Matching : Types, Principle, Procedure and Interpretation