Who can forget their jolly childhood days? We played with our friends in the playground, and we ran all around the house. What a time it was. However, sometimes while playing, we suffered injuries and wounds. Of course, those wounds healed, but then some wounds left scars. You would still find these scars where the damage was 30 years ago. But the good news is that it stopped scarring. Imagine a disease in which this process of forming a scar never ends. The hard tissue that is the scar keeps growing beyond the margins of the wound and forms a solid lump. Indeed, this is what happens in a fibrotic disease of the skin called keloids 1, 2. This excessive scarring of the tissue leads to tissue hardening and hence loss of function and it is termed fibrosis 3.
All organs scar and develop fibrosis in response to an injury
Nevertheless, the skin is not the only organ that gets injured and scarred. For instance, after a heart attack, the heart tissue suffers damage because some cells die due to a lack of oxygen. It starts the healing process and forms a scar in the heart 4. The hardening of the heart tissue hampers its functioning, weakens the heart and makes you prone to cardiac arrest and death. High glucose levels in the blood also damage tissues owing to glycemic injury. This is the major cause of cardiovascular disease, diabetic nephropathy (renal fibrosis), and other secondary ailments in diabetic patients 5. Sometimes, we injure our own organs due to lifestyle choices. For example, when we smoke, we wound our lungs and put ourselves at risk of developing lung fibrosis 6. When we drink too much, we harm our liver which is the cause of liver fibrosis (liver cirrhosis) 7. Lifestyle choices and high blood pressure (hypertension) can amplify the usual wear and tear that happens in arteries. The atrial damage causes fibrotic plaques to form inside the blood vessels, a disease commonly known as atherosclerosis 8. Then there are some disease-causing germs which cause injury to organs. Take Covid-19 as an example. People who suffer from severe Covid-19 suffer massive damage to their lungs. Hence, one of the concerns for severe Covid-19 patients even after their recovery is the development of lung fibrosis which can cause long-term lung dysfunction 9, 10.
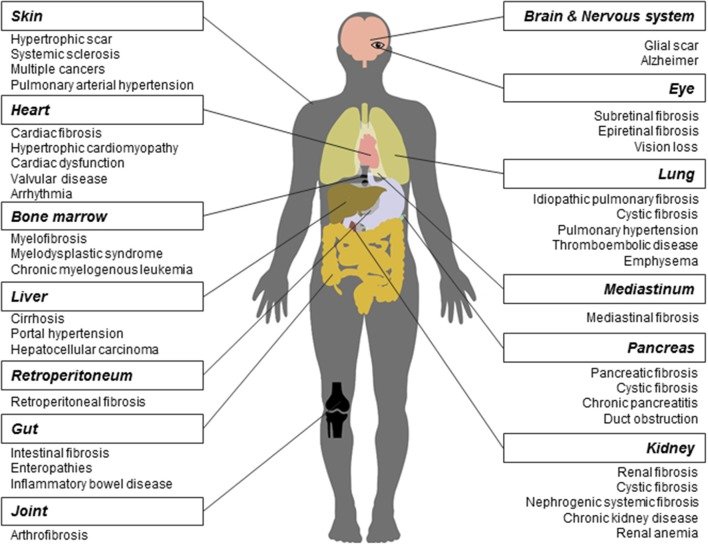
Reproduced from Li et al., 2017. Front. Pharmacol. 8:855.11. CC BY 4.0
However, it does not always have to be a heart attack, a pathogen, a lifestyle choice, or a lifestyle disease like diabetes that initiates fibrosis. Sometimes, it can start because there are dysregulated molecular signals that mimic the wound-healing response, without having any actual wound, anywhere. Or it can happen due to an autoimmune disorder, in which immune cells attack and damage the body’s own tissues. An example of such a fibrotic disease is scleroderma (also known as systemic sclerosis) 12, where the fibrosis starts in the skin in the extremities of the limbs(fingers and toes) and then spreads to other organs – lungs, heart, and kidneys.
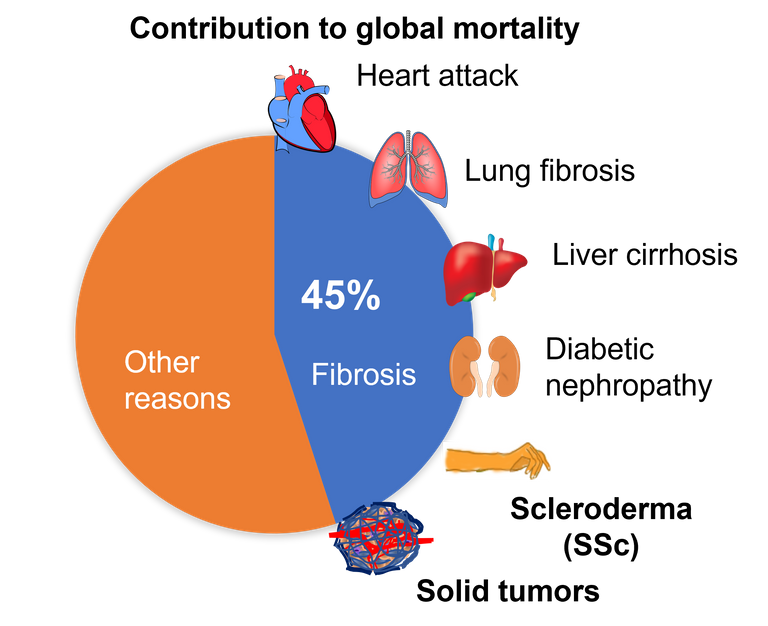
Overall, fibrosis is either a cause or a consequence of many chronic diseases. Even, the tissue surrounding the cancerous tumour, known as tumour stroma, is a hard-fibrotic tissue, which nurtures the tumour and helps cancer to spread 13, 14. Overall, fibrosis is the cause of 45% of deaths that occur worldwide 3. And yet, we have no cure for fibrosis. However, if we try to understand how a wound heals and what goes wrong that sometimes the scarring does not stop, then we can come up with solutions.
A brief look into the wound-healing.
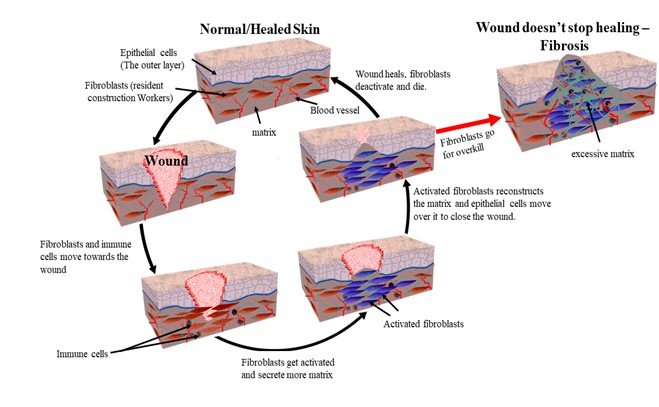
Let us take an example of a skin wound. As soon as you cut your skin, the first response of your body is to limit the blood flow. The blood vessels constrict, and the clotting factors in the blood get activated and form a clot. A few hours later, the blood vessels dilate, allowing immune cells like neutrophils and macrophages to enter the wound site. Their job is to clear up the damaged cells and fight any invading bacteria that might have entered the wound. Then comes the resident construction workers of the skin – fibroblasts – who live in the bottom layer of the skin called the dermis. Their typical job is to make the matrix for the tissue. The tissue matrix is like cement that holds the tissue together. When they see a wounded tissue around them, they become hyperactive in producing and secreting this matrix 15.
The epithelial cells which form the top layer of the skin visible to us then migrate over this matrix to close the wound. Meanwhile, the fibroblasts continue to organise the matrix secreted by them. They aim to restore the architecture of the tissue. After restoration, the fibroblasts deactivate, or they die. This organisation of the matrix can go on for years. And this is what that 30-year-old scar you have is all about. However, in some cases, these construction workers go for overkill. That is, they remain hyperactive and keep producing the matrix, leading to the development of fibrotic disease 3.
The healing process is similar in all organs across the body and shares common cellular and molecular pathways. And at the centre of all fibrotic diseases are these construction workers – the fibroblasts. The key here is to understand the nature of these construction workers and why they stay constitutively active in fibrotic diseases. Are there false signals that are telling the fibroblasts to remain active? Are there dysregulated immune cells causing more damage to the tissue before it can heal? Or is there something intrinsically wrong with these fibroblasts? In order to answer these questions we needed a mouse model which can mimic a human fibrotic disease.
Creating a disease model for human fibrotic skin disease scleroderma.
We know that the foetal wounds do not scar, but adult wounds do 16. The mouse skin repair perfectly, but human skin form scars. We noticed that there is a protein called Snail which expressed in skin epithelial cells of adult humans when they are wounded, but this does not happen in the mouse. Moreover, we found that this protein is expressed in skin epithelial cells of patients with skin fibrosis (scleroderma), but not in healthy people. So, we created a mouse via genetic manipulation, such that it constitutively expresses this protein in the epithelial cells as human skin fibrosis patient do? Will they scar if we wound them? They do, just as we predicted. But what was more interesting is that they scarred all over the body even without a wound. These mice displayed all the known symptoms of human fibrotic skin disease - scleroderma. The fibrosis started developing in the skin of extremities (tail and limbs), and it spread throughout the body and internal organs and these mice as they aged.
Using this mouse model we found interesting targets for for developing novel therupatics for scleroderma. But more on that later. I will describe our findings in more details in part 2. Meanwhile, if you are interested to read it you can read our recently published paper in JID in which I am a co-first authror.
Paper on which the blog is based
#STEMsocial powered by Hive
Video by @gtg
References
About contacting me
You can reach out to me on discord if you are in stemsocial discord. Or you can even send me a DM. My discord handle is the same as my hive - @scienceblocks. You can also ping me on my telegram handle: @UncertainHeisenberg. Or follow me on Twitter: @scienceblocks1
I have added @mycrimsonhues and @gtg as 1% beneficaries as token of thanks for helping with the illustrations and stemsocial video used in this post, respectively.