Meningitis is one of the most common clinical presentations in Sub-saharan Africa, especially in children. I have seen a lot of cases personally in the clinic & ER and have been part of the management team of many. Meningitis exerts a heavy burden on health care in Sub-Saharan Africa.
Meningitis is observed worldwide but the highest burden of the disease is in the meningitis belt of sub-Saharan Africa, stretching from Senegal in the west to Ethiopia in the east. Around 30,000 cases are still reported each year from that area.
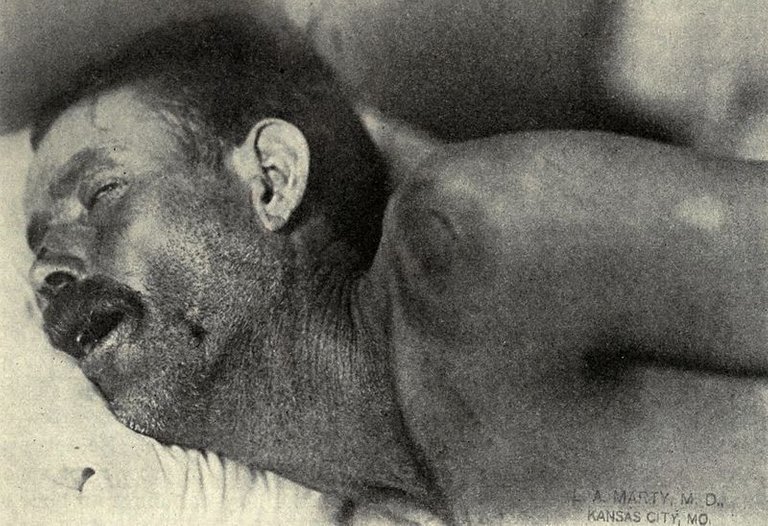
Neck stiffness, Texas meningitis epidemic of 1911–12. By L.A. Marty, M.D, Kansas City - Sophian, Abraham: Epidemic cerebrospinal meningitis (1913), St. Louis, C.V Mosby (Scan from archive.org)., Public Domain, Link
What is Meningitis
What then is the sub-arachnoid space? To understand that, we must first understand the Meninges.
The meninges refer to the membranous coverings of the brain and spinal cord. There are three layers of meninges, known as the dura mater, arachnoid mater and pia mater.
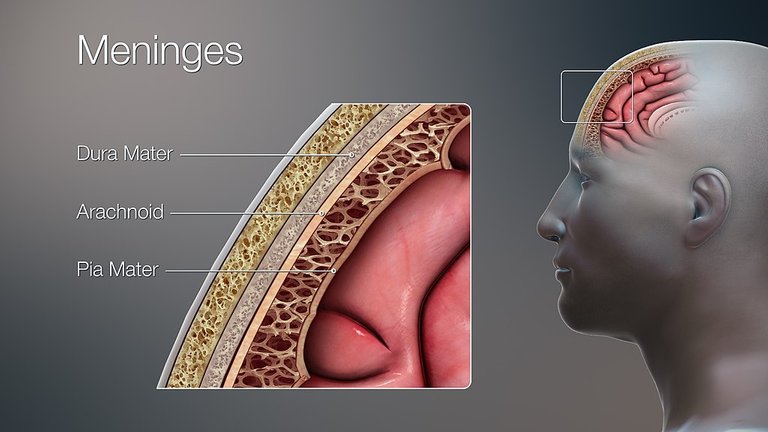
A detailed depiction of different layers in skull using a 3D medical animation still image, with special focus on different layers of Meninges. By Scientific Animantions - CC BY-SA 4.0, Link
The meninges have a lot of functions. The most important though is that they reflect infection of the arachnoid mater and the cerebrospinal fluid (CSF) in both the subarachnoid space and in the cerebral ventricles.
The meninges, subarachnoid space and brain parenchyma are all frequently involved in the inflammatory reaction when there is an ongoing infection. (meningoencephalitis)
The most common type of Meningitis is Bacterial Meningitis. This is the most often presented case of meningitis in the clinics.
Bacterial Meningitis
Bacterial Meningitis
The highest incidence is among neonates, who are usually infected by bacteria found in the birth canal at the time of parturition. Group B streptococci (Streptococcus agalactiae) account for the majority of cases; other causes include Listeria monocytogenes, E.coli, other Gram-negative bacilli, and enterococci.
From age, 1 to 23 months, the most common organisms are Streptococcus pneumoniae and Neisseria meningitidis
Children from 2 - 5 years used to have a high rate of infection caused by Haemophilus influenzae type B. However, the wide use of protein-polysaccharide-conjugated vaccines has dramatically reduced the incidence of this infection.
From age 2 through 18, N. meningitidis is the most common cause, accounting for more than 1/2 of cases, followed by S. pneumoniae
In adults up to age 60, S. pneumoniae is the most common followed by N. meningitis.
Over age 60, most cases are due to S. pneumoniae and less often L. monocytogenes
Epidemiology
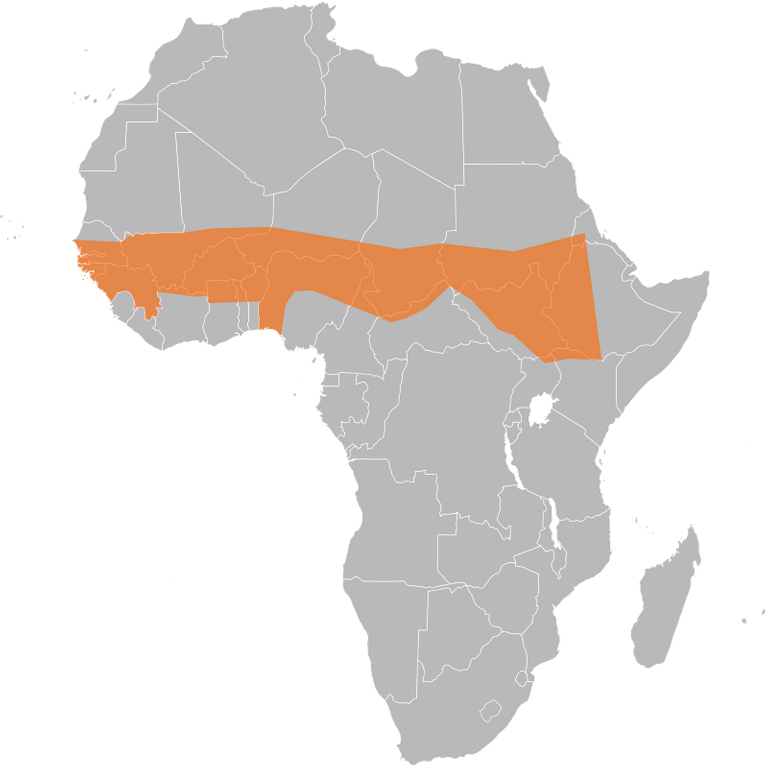
The meningitis belt, showing the distribution of meningococcal meningitis in Africa. By Ninjatacoshell, CC BY-SA 3.0, Link
In the meningitis belt, serogroup A has historically accounted for 90% of meningococcal disease cases and the majority of large-scale epidemics. In the past, Nigeria has suffered large-scale outbreaks of meningitis A. In 2009, such an outbreak in the country caused over 55,000 cases with close to 2,500 deaths.
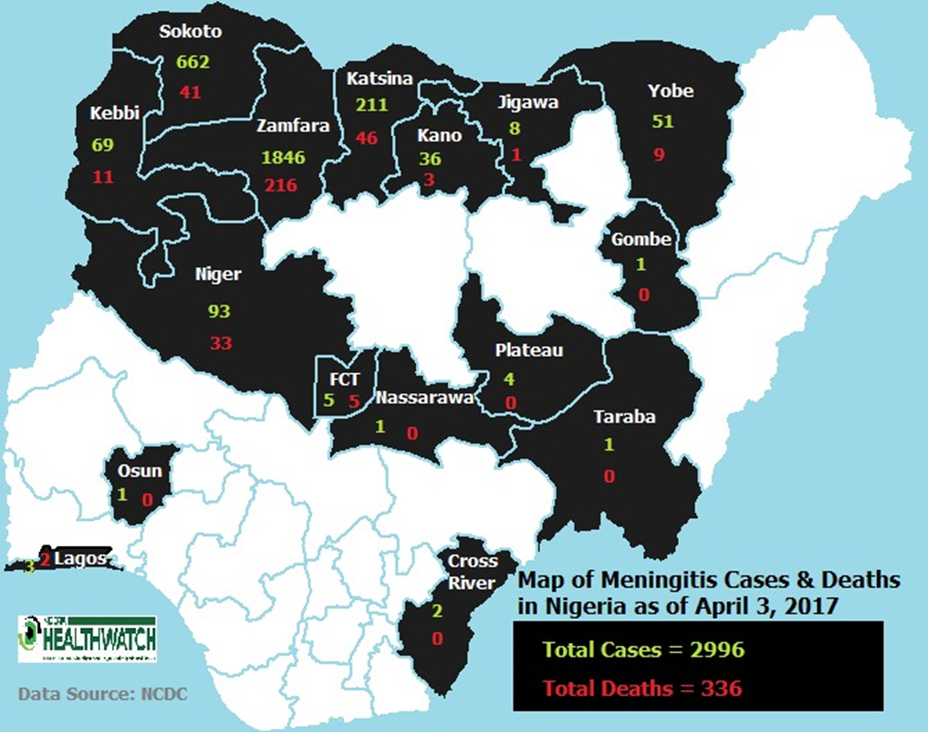
Source: Nigeria Center for Disease Control
The rates of meningococcal disease are highest in young children because of their reduction of protective maternal antibodies and then increase again for adolescents and young adults
Risk Factors
Some of the risk factors of Bacterial Meningitis include:
- Young age
- Dry season
- Close contact with a case of meningococcal disease
- Sharing a bite of food, a drink, utensils, or any activity where respiratory secretions, throat secretions, and saliva are exchanged
- Overcrowding
- Active or passive smoking
- Co-infections of respiratory pathogens.
- Complement deficiencies.
- Defects in sensing or opsonophagocytic pathways
- Splenic dysfunction (sickle cell anaemia or asplenia) increased risk of pneumococcal, H.influenza type B, rarely meningococcal sepsis and meningitis.
- Head trauma or neurosurgical procedures (staphylococci).
- Neural tube defects
Pathophysiology
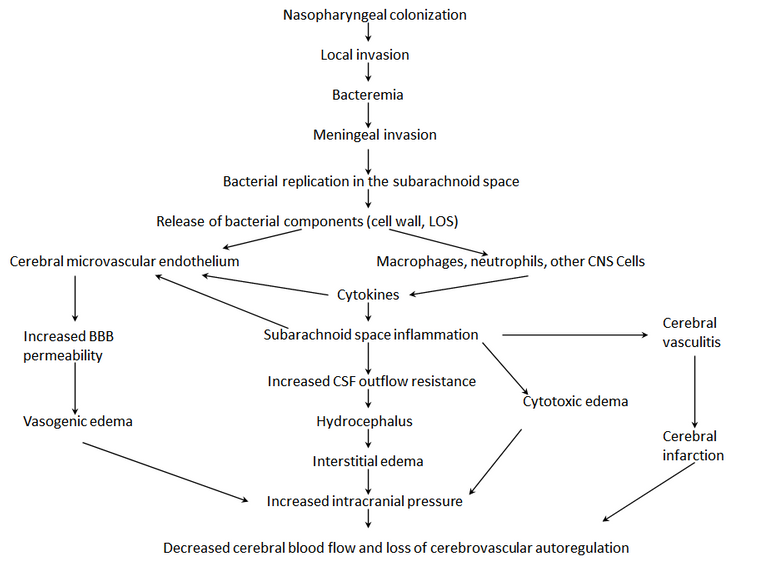
Original Image created by @gamsam
Signs and Symptoms
- Severe headache - A person with meningitis may describe the headache as the worst one they’ve ever had.
- High fever - The infection can cause a high fever (39°C or over) which does not get lower with a tepid bath or fever-reducing medicine.
- Neck stiffness - Swelling in the meninges (membranes around the spinal cord and brain) causes a stiff neck that makes it extremely painful to move the neck or head.
- Nausea and vomiting - Vomiting is common with many illnesses. However, if vomiting happens with the other symptoms listed, it may be caused by meningitis.
- Numbness or loss of feeling - Sepsis (also known as blood infection) can reduce the amount of blood that gets to a person’s hands and feet, causing numbness, coldness, or loss of feeling.
- Photophobia (Light Sensitivity) - A person with meningitis may find it painful to look at bright lights, and will try to avoid them.
- Confusion - Swelling around the brain can make a person confused and seem "out of it.“
- Rash - Purple spots called PURPURA FULMINANS that do not turn white when you press on them is a sign of sepsis (also known as blood poisoning).
- Seizures - Sometimes people with meningitis have seizures similar to the kind that people with epilepsy have.
- Meningismus - a state of meningeal irritation with symptoms suggesting meningitis that often occurs at the onset of acute febrile diseases, especially in children.
- Kernig Sign - The test for Kernig sign is done by having the person lie flat on the back, flex the thigh so that it is at a right angle to the trunk, and completely extend the leg at the knee joint. If the leg cannot be completely extended due to pain, this is Kernig sign.

Kernig's sign in a case of cerebrospinal meningitis. Note the contractures of ham-string muscles, the retraction of the head, the expression of suffering produced by the examiner's effort to extend the lower leg, and the pronounced emaciation. (Harlem Hospital, Dr. R. G. Wiener). By R. G. Wiener, Harlem Hospital - Sahli, H. A treatise on diagnostic methods of examination (translation from the fourth revised & enlarged German edition). Saunders. 1909., Public Domain, Link
- Brudzinski Sign - The Brudzinski's sign is positive when passive forward flexion of the neck causes the patient to involuntarily raise his knees or hips in flexion.
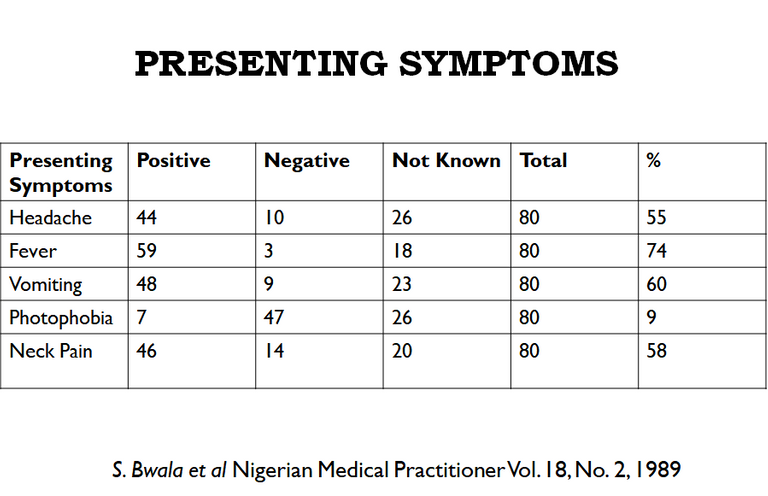
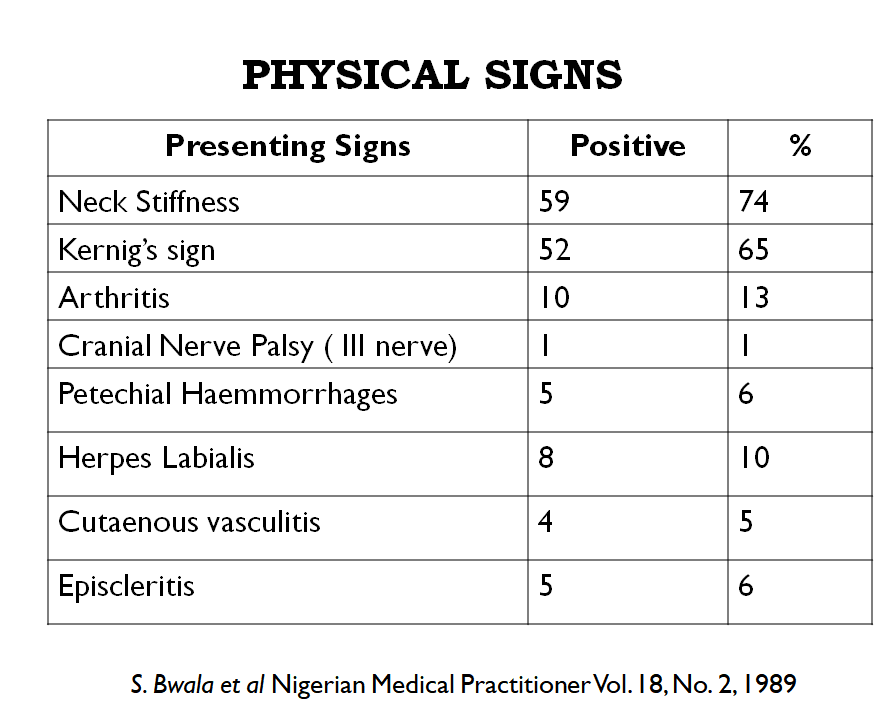
Incidence of Signs and Symptoms
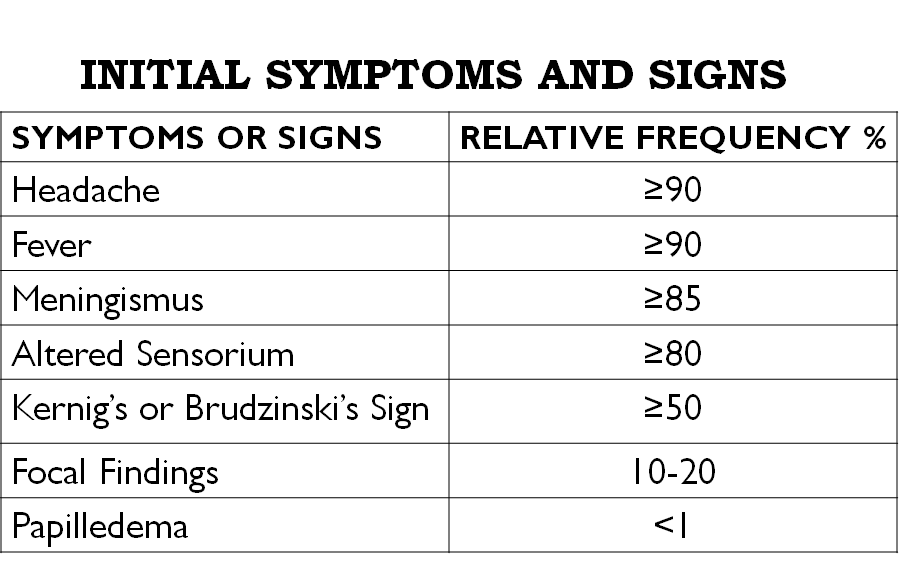
Data collected from the University of Port Harcourt Teaching Hospital. Image made by @gamsam
Complications
Up to 10 percent of people with bacterial meningitis don't survive. Some who survive the illness may come down with serious complications which may include:
- Seizures
- Brain damage
- Hearing loss
- Disability
- Hydrocephalus
- Subdural effusion or empyema
- Stroke
- Abscesses
- Dural sinus thrombophlebitis - this is the presence of a blood clot in the dural venous sinuses, which drain blood from the brain.
Mortality Rate and Prognosis
Prevention
- Vaccines
- Chemoprophylaxis
- Avoiding overcrowded places.
- Sleeping in well-ventilated places.
- Avoiding close and prolonged contact with a sick person.
- Properly disposing of respiratory and throat secretions.
- Strictly observing hand hygiene and sneezing into elbow joints/ sleeves.
- Reducing handshaking, kissing, sharing utensils or medical interventions such as mouth resuscitation.
- Getting vaccinated with a relevant vaccine.
- Avoiding self-medication.
- Avoiding smoking
Davidson's Principles and Practice of Medicine - 24th Edition
Meningococcal meningitis [Internet]. Who. int. World Health Organization: WHO; 2018.
The Meninges - Dura - Arachnoid - Pia - TeachMeAnatomy [Internet]. Teachmeanatomy.info. 2019.
Meningococcal [Internet]. Centers for Disease Control and Prevention. 2019.
Bacterial Meningitis [Internet]. Department of Neurology.
There are vaccines against Haemophilus influenzae type b (Hib) and against some strains of N. meningitidis and many types of Streptococcus pneumoniae.
The vaccine against Haemophilus influenza (Hib) has reduced Hib meningitis cases by 95 per cent since 1985. There are vaccines to prevent meningitis due to S. pneumoniae.
The pneumococcal polysaccharide vaccine is recommended for all persons over 65 years of age and younger persons at least 2 years old with certain chronic medical problems.
Meningococcal vaccines are active against many strains of N. meningitidis. The majority of meningococcal infections in Nigeria were caused by type B meningococcus. The present menigitis C epidemic is not new and a vaccine is available.
There is a role for chemoprophylaxis to prevent the spread of meningococcal and Haemophilus meningitis but not for pneumococcal disease.
The use of antimicrobial therapy to eradicate pharyngeal carriage of meningococci is widely accepted to prevent the development of disease in close contact and to eradicate pharyngeal carriage.
Drugs like Rifampin, Ceftriaxone and Ciprofloxacin have proven to be effective.
Other forms of prevention not directly related to the causative agents include:
Conclusion
References


Check out my other recent finance posts:
Check out my other non-finance posts:

Written by @gamsam
All images used are taken by me and copyright free