There are signs, but obviously at some point, you will likely end up seeking care at a medical office, and they will test you anyways.
But what if pregnancy tests just are available in my parts? What happens then, and what will happen afterwards?
In that case... look for these signs:
Presumptive Signs
- Amenorrhea
- Nausea/vomiting, typically in the morning, during the first trimester
- Breasts swelling and tenderness
- Fatigue
- Urinary frequency
- Increase in basal body temperature
- Quickening - fetal movements at 16 weeks or 4 months (early 2nd trimester)
Probable Signs
- Cervical softening at 4 weeks, known as Goodell's Sign
- Blue color of the cervix and vagina at 6-8 weeks, known as Chadwick's sign
- Softening of the uterine isthmus at 6-8 weeks, known as Hegar's sign
- Enlarging uterus
- Fetus bounces back when pushed, known as Ballottement
- Urine or blood pregnancy tests to tests for hCG
Positive Signs
- Palpation of the fetus
- Ultrasound and visualization of the fetus
- Fetal heart tones using a doppler at 10-12 weeks or at 20 weeks with a stethoscope
However, here lies the problem if you think you may be pregnant... HOW FAR ALONG AM I?
Without an ultrasound or without knowing the exact date of your last menstrual period, you will have to rely on measuring the fundal height.

Fundal Height
At 12 weeks or the third month:
- Uterine fundus has risen above the symphysis pubis
- Fetal heart tones can be heard by the Doppler
At 16 weeks or the fourth month:
- Uterine fundus is now between the symphysis pubis and the umbilicus
At 20 weeks or the fifth month:
- Uterine fundus is level with the umbilicus
- Fetal heart tones can be heard by a stethoscope
Between 20-35 weeks:
- Fundal height in centimeters equals the number of weeks of gestation
- Measure the distance between the pubic symphisis and the top of the uterine fundus using a tape measure.
Discrepancies:
- If there is a difference of 2cm or more for uterine size vs weeks gestation, then an ultrasound is required.
Changes to the Mother's Body During Pregnancy
Cardiac:
- Heart shifts forward and left
- Heart rate increases by 15 to 20 bpm
- Heart sounds become louder
- S3 heart sound is common
- Wide splitting of S1 sound
- S2 splitting may be heard in the 3rd trimester
- Systolic murmur of grad II/IV over the pulmonary and tricuspid areas is common
- A mammary souffle is heard over the breasts in late pregnancy and during lactation
- Cardiac output increases 30-50%
- Systemic vascular resistance decreases, therefore systolic BP also decreases
- Plasma volume increases by 50%
- Increased risk for anemia due to hemodilution
- Preload increases because of higher blood volume
- Afterload decreases because of lowered systemic vascular resistance
- Systolic and diastolic BP decreases in the first and second trimester, allowing hypertensive mothers to wean off blood pressure medication during this time.
- However, by the third trimester, the blood pressure returns, but ACEI and ARBS are contraindicated in pregnancy, so methyldopa (Aldomet) or labetalol (Normodyne) are frequently used.
- An enlarged uterus can compress the Vena Cava, leading to decreased blood flow back to the brain, causing dizziness.
- Pregnancy can cause increased coagulability.
Lungs:
- Basal rales that disappear with coughing or deep breathing
- Breathlessness and decreased exercise tolerance
- The uterus pushes up the diaphragm as it gets larger
- Total lung capacity drops slightly
Thyroid:
- Grows up to 15% larger, with higher metabolic activity
Gastrointestinal:
- Decreased peristalsis due to progesterone
Integumentary System:
- Pigment increases in melanocyte-stimulating hormone due to higher levels of estrogen.
- Leads to linea nigra, which is a dark line that runs from the mons pubis to the ubilicus midline.
- Nipples and areola darken
- Chloasma/Melasma - Blotchy hyperpigmentation on forehead, cheeks, nose, and upper lip; Regresses within 1 year, but sometimes permanent
- Striae Gravidarum (stretch marks) - commonly found on abdomen, breasts, and thighs
- Telgen Effluvium (Hair loss) - During the postpartum period, hair loss may accelerate, but is temporary
Renal System:
- Kidney size increases during pregnancy
- Glomerular filtration rate is higher due to higher cardiac output and renal blood flow
Ear, Nose, and Throat:
- Nasal congestion and sometimes bloody nose due to increased blood flow to the nasopharynx
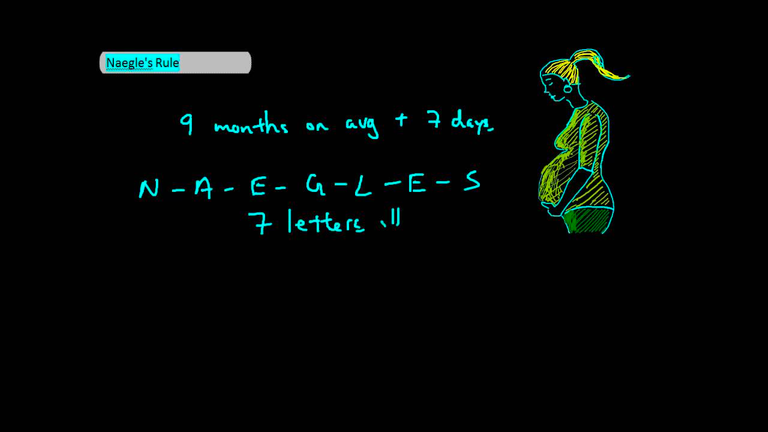
Naegele's Rule
- Estimates date of delivery during the first trimester
- Not useful for irregular menstrual cycles
- Method 1: LMP + 9 months + 7 days
- Method 2: LM - 3 months + 7 days
Obstetric Terminology
G - Gavida - Number of Pregnancies (twins or multiples count as one pregnancy)
T - Term - Number of delivers after 37 weeks
P - Preterm - Number of deliveries after 20 weeks (up to 38 weeks)
A - Abortion - Number of delivers before 20 weeks (induced or spontaneous)
L - Living - Number of living children
Postpartum - Occurs immediately after delivery and lasts about 6 weeks
Uterine Involution
- Normal for postpartum women to have uterine contractions (spontaneous or with breastfeeding) during the first 2-3 days after giving birth.
- After delivery, the uterus is the size of a 20-week pregnancy, with the fundi located at the umbilicus
- Lasts 6 weeks.
Diseases During Pregnancy
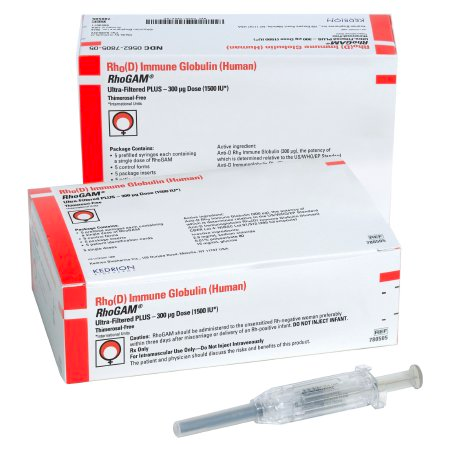
Rh-Incompatibility Disease
- For Rh-negative mothers with Rh-positive fetuses - maternal immune system develops antibodies against Rh-positive blood if not given RhoGAM (gamma globulin against Rh factor).
- Give RhoGAM for all pregnancies of Rh-negative mothers - even if they terminate in miscarriages, abortions, or tubal or ectopic pregnancies.
RhoGAM
- Anti-D immune globulin made from pooled IgG antibodies against Rh (rhesus) factor.
- Helps prevent maternal isoimmunization or alloimmunization.
- If RhoGam is not given to Rh-negative pregnant women, this will result in fetal hemolysis and fetal anemia in future pregnancies.
- Coombs test - detects presence of Rh antibodies in the mother (indirect Coombs test) and the infant (direct Coombs test).
- RhoGam 300 mcg intramuscular is first given at 28 weeks gestation.
- Second dose given within 72 hours after delivery.
- RhoGam decreases the risk fo isoimmunization of the maternal immune system by destroying fetal Rh-positive RBC's that have crossed the placenta.
Gestational Diabetes Mellitus (GDM)
- GDM places mothers at high risk for diabetes type 2
- High rates of reoccurrence in future pregnancies
- Higher rates of neural tube defects, congenital heart disease, birth trauma, preeclampsia, and neonatal hypoglycemia
- Screened at first visit, and if not high risk, screen at 24 to 28 weeks gestation
- Screening is diagnosed in the second to third trimester:
One-Step Method
- Check fasting glucose
- Administer 75 gram oral glucose tolerance test
- Check glucose in 1 hour
- Check glucose at 2 hours
Diagnostic Criteria:
- Fasting: equal or >92 mg/dL
- 1 hour: equal or > 180 mg/dL
- 2 hour: equal or < 153 mg/dL
Two-Step Method
- Non-fasting 50 gram glucose load
- Check plasma glucose at 1 hour
- If 140 mg/dL or higher, rule out GDM by ordering a 100 gram OGTT (oral glucose tolerance test)
Diagnostic Criteria:
- Fasting: equal or > 95 mg/dL
- 1 hour: equal or > 180 mg/dL
- 2 hour: equal or > 155 mg/dL
- 3 hour: equal or > 140 mg/dL
GDM Treatment Plan:
Glycemic targets are:
- Preprandial: 95 mg/dL or less
- 1-hour postmeal: 140mg/dL or less
- 2-hour postmeal: 120mg/dL or less
- A1C goal: 6-6.5%
Action: - Small frequent meals and exercise
- Perform frequent glucose monitoring at home (four to six times a day)
- Insulin injections needed if unable to control blood glucose by self
- Metformin and glyburide may be prescribed
- Test for GDM 6-12 weeks postpartum and at least every 3 years afterwards

Urinary Tract Infections (UTI's)
- Also known as acute cystitis, typically presents with dysuria, frequency, urgency, and nocturia.
- Can lead to preterm birth and low birth weight.
Asymptomatic Bacteriuria
- Requires treatment due to high risk for acute pyelonephritis.
- Obtain urine sample before antibiotic treatment and after.
Can treat with Augmentin, Amoxicillin, Cephalexin, and Fosfomycin. However, a note regarding nitrofurantoin:
Nitrofurantoin and Sulfa Drugs
- Avoid near term i.e. 38-42 weeks, during labor, and during delivery.
- Increases the risk of hyperbilirubinemia, which can cause kernicterus
- Do not use if G6PD anemia is suspected, as it can cause hemolysis
- Can cause pulmonary reactions, liver damage, neuropathy and others
Miscarriages aka Abortions
Spontaneous Abortion - loss of fetus before 20 weeks
Threatened Abortion - vaginal bleeding occurs, but cervical os remains closed. Most will result in ongoing pregnancy.
Inevitable Abortion - Cervix is dilated and unable to stop process. Fetus will be aborted.
Complete Abortion - Vaginal bleeding with cramping occurs. Placenta and fetus are expelled completely. Cervical os will close and bleeding stops.
Incomplete Abortion - Vaginal bleeding with cramping occurs. Placental products remain in the uterus. Cervical os remains dilated and bleeding persists. Vaginal discharge is foul smelling. Treatment is dilation and curettage and antibiotics.
Preeclampsia, Placenta Abruptio, and Placenta Previa I discussed in an earlier article. Please refer to that one for more details. Join me next time, as I discuss postpartum care and all the good things that come with it.