According to Merriam-Webster, the word, Endocrine, was first used in 1914 as an adjective, and then in 1922 as a noun.
Inspired from the French words, "holocrine" and "merocrine", French histologist Édouard Laguesse coined the term "endocrine" to describe "internal secretion".
But, what does it compose of? And why should we care?
Endocrine system is mainly composed of:
- The Hypothalamus found in your brain
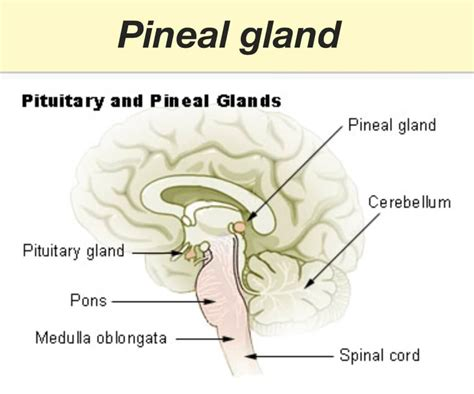
- The Anterior and Posterior Pituitary, also found in your brain, but lower
- Target organs, which include your thyroid, ovaries or testes, adrenal cortex, your uterus if you have one, your kidneys, your pineal gland, and your breasts if you have them - all of which are in various places.
Hypothalamus
Like I said earlier, is located above the midbrain, but below the thalamus. The hypothalamus directs the nervous and endocrine system by signaling the pituitary gland. It's part of the HPA axis. It acts to stimulate or suppress pituitary hormones.
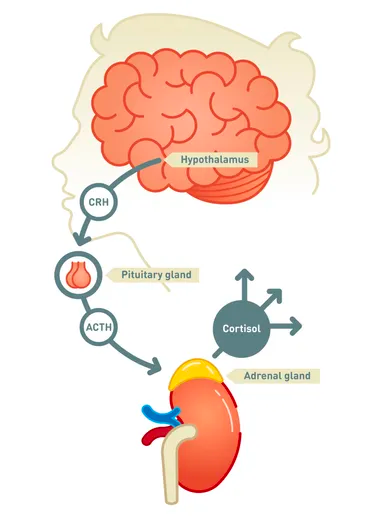
Pituitary Gland
Located at the base of the brain is stimulated by the hypothalamus to produce the hormones FSH, LH, TSH, adrenocorticotropic hormone (ACTH), and growth hormone (GH). All of which act on different target organs that we'll discuss later.
Anterior Pituitary Gland (Adenohypophysis)
The pituitary gland is subdivided into anterior and posterior, and the anterior produces the following hormones:
- FSH (follicle-stimulating hormone) - stimulates the ovaries to produce follicles/eggs, and stimulates estrogen production
- LH (luteinizing hormone) - stimulates the ovaries to ovulate, produces progesterone via the corpus luteum, and stimulates the testicles to produce testosterone
- TSH (thyroid-stimulating hormone) - stimulates the thyroid gland to produce T3 and T4
- GH (growth hormone) - stimulates somatic growth of the body
- ACTH (adrenocorticotropic homrone) - stimulates the adrenal glands to produce glucocorticoids (cortisol) and minneralocorticoids (aldosterone)
- Prolactin - for milk production and lactation
- Melanocyte-stimulating hormone - to produce melatonin in the presence of UV light (typically 11pm - 3am)
Posterior Pituitary Gland
Doesn't produce hormones, but stores two hormones made by the hypothalamus:
- Antidiuretic hormone (vasopressin)
- Oxytocin
Thyroid Gland
Located below the thyroid cartilage, is stimulated by TSH from the pituitary gland to produce T3 and T4.
Parathyroid Glands
Located behind the thyroid glands, and produces parathyroid hormone (PTH). PTH regulates the calcium level in the blood by leeching or increasing absorption of calcium from the bones, kidneys and GI tract.
Pineal Gland
Important to note this is not part of the pituitary, but produces melatonin, which regulates the circadian rhythm.
Diseases to Watch Out For
Hypoglycemia - blood glucose less than 50mg/dL, presenting with weakness, tremors, difficulty focusing, and typically occurs in those with Type I diabetes. Can progress to coma.
Type I diabetes - typically starts young with a presentation of constant thirst, frequent urination, and weight loss despite constantly eating. Breath will have a fruity odor, and there will be a presence of broken down fats i.e. ketones in the urine.
Thyroid Cancer - nodules can form on the thyroid, usually on the upper half, which will swell and become painful. It will also cause hoarseness of the voice and difficulty swallowing.
Thyroid storm (thyrotoxicosis) - heart rate, blood pressure, and temperature are elevated to dangerously high levels, which can cause decreased level of consciousness, fever, and abdominal pain. Life threatening.
Myxedema - severe hypothyroidism, which causes cognition to be slowed and depression, dementia, low blood pressure, and hypothermia to set in.
Pheochromocytoma - rare adrenal tumor that can cause random headaches, sweating, fast heart rate and high blood pressure. Foods high in tyramine, such as found in cheese, beer, wine, chocolates, dried meats - basically anything good in life, and in MAOI medications can trigger this.
Hyperprolactinemia - slow pituitary tumor that can cause lack of periods, production of breast milk in men and women, and headaches and vision changes if large enough.
Diseases Under Management
Primary Hyperthyroidism (Thyroitoxicosis)
- low or undetectable TSH and high T4 and T3 levels
- most common cause is an autoimmune disorder, Grave's Disease
Grave's diseases
- most common cause of hyperthyroidism, in which the autoimmune disorder causes hyper-functioning of the thyroid gland, producing excess T3 and T4.
- Presents with sometimes a goiter, fine tremors in the hands, exophthalmos, fast heart rate, atrial fibrillation, congestive heart failure, fine hair, brisk reflexes.
- Can trial propylthiouracil (PTU) or methimazole (Tapazole) to shrink the gland, and beta blockers, such as propranolol to manage the symptoms
- Note Armour thyroid is made fro dried pig thyroid glands, which contain both T3 and T4.
- Drugs, such as lithium, amiodarone, high doses of ioddine, dopamine, and interferon affects the thyroid.
- All with hyperthyroidism should be referred to an endocrinologist.
Primary Hypothyroidism
- high TSH with low free T4 levels
- common causes include Hashimoto's thyroiditis, postpartum thyroiditis, thyroid ablation/surgery/radiation, with Hashimoto's as the most common cause
Hashimoto's Thyroiditis
- Chronic, autoimmune disorder, where the body produces antibodies (TPO) that destroys the thyroid gland.
- Treatment includes levothyroxine (Synthroid), and recheck TSH every 6-8 weeks until TSH is at normal level. When normal, check every 12 months.
- Synthroid should be crushed in the mouth before swallowing, and should be taken on it's own an hour before food or other medications.
Diabetes
Metabolic disorder that affects metabolism of carbohydrates and fat, in which if uncontrolled can cause vascular damage leading to the destruction of the nervous system, immunity, and can result in amputations.
Type I diabetes
B-cells of the pancreas are destroyed, leaving the body unable to produce insulin. Therefore, the body will switch over to using fat for fuel. Ketones as a byproduct will build up in the body, and if it builds up enough, can cause diabetic ketoacidosis and possibly coma and death.
Type II diabetes
Insulin secretion from the pancreas progressively has to secrete more due to insulin resistance. This is a sign of too much sugar in your bloodstream. Risk factors include:
- obesity or overweight above a BMI of 25
- abdominal fat
- being sedentary
- race
- genetics
- metabolic syndrome, which is a triad of either obesity, high blood pressure, high cholesterol levels, or high blood sugars.
**Criteria for the Diagnosis of Diabetes include:
**- A1C test of over 6.5% (percentage of blood sugar attached to cells over 3 months)
- fasting blood glucose more than 126 mg/dL
- symptoms of diabetes, such as constant thirst, urination, and consumption of food
- an oral glucose tolerance test of 200 mg/dL after the 2 hour mark, after consumption of 75 grams of Glucola
Dawn Phenomenon
- Due to hormones, blood sugar spikes between 4-8am, and the diabetic wakes up with elevated blood sugars
Somogyi Effect (Rebound Hyperglycemia)
- Nocturnal low blood sugar stimulates the hormone, glucagon, to elevate blood sugar, resulting in high blood sugar by 7am.
- Due to over-treatment of bedtime insulin.
- Treat by eating a snack before bedtime or lower bedtime insulin dosage
Diabetic Retinopathy
- Neovascularization, miciroaneurysms, cotton-wool spots, and exudates found on retina of the eye. If found, will require referral to an ophthalmologist, and an eye exam every 6-12 months.
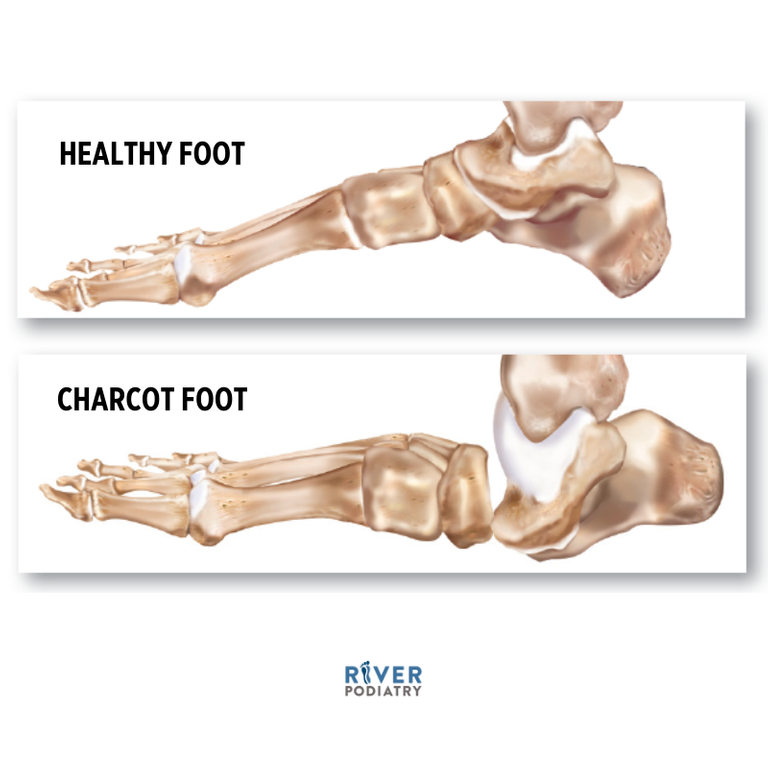
Charcot's Foot and Ankle (Neuropathic Arthropathy)
-deformity of the foot due to joint and bone dislocation and fractures due to loss of sensation of the foot and ankle.
Diabetic Medications
Biguanides, such as Metformin
- decreases gluconeogenesis and decreases insulin resistance
- rarely causes hypoglycemia
- may cause GI upset, but continue to take, as the GI will begin to tolerate
- Monitor renal and liver function
- hold metformin on day of procedure and 48 hours afterwards if the procedure uses IV contrast dye
Sulfonylureas, such as glipizide
- stimulates the beta cells of the pancreas to produce more insulin
- risk for hypoglycemia and photosensitivity
- monitor renal and liver function
- can cause weight gain
Thiazolidinediones (TZD's), such as pioglitazone (Actos)
- enhances insulin sensitivity in muscle tissue and reduces gluconeogenesis
- can combine with metformin, glipizide, GLP-1, SGLT2, DPP-4, and insulins
- DO NOT USE in patients with congestive heart failure, as it causes water retention
- Avoid use if there is a history of bladder cancer, liver disease, DMI, and pregnancy
Bild-Acid Sequestrants, such as Questran, Welchol, and Colestid
- reduces hepatic glucose production and may reduce intestinal absorption of glucose
- may cause upset stomach
Meglitinide (Glinides), such as Prandin and Starlix
- stimulates pancreatic secretion of insulin
- may cause low blood sugar
Alpha-Glucosidase Inhibitor
- slows intestinal carbohydrate digestion and absorption
- does not cause low blood sugar
- can cause GI upset
Incretin Mimetics or Glucagonlike Peptide (GLP-1) Mimetics, such as Byetta or Victoza
- stimulates GLP-1, which increases insulin production and slows glucose release after eating
- can contirubte to weight loss and appetite supression
- does not cause low blood sugar
- may cause pancreatitis and avoid in persons with a history or family history of thyroid cancer
Sodium-Glucose Cotransporter-2 (GLT2) Inhibitors, such as Invokana, Farxiga, and Jardiance
- blocks glucose reabsorption by the kidney
- does not cause low blood sugar
- risk for DKA, UTI's, and amputations
- causes weight loss and low blood pressure
Dipeptidyl Petidase-4 (DPP-4) Inhibitors, such as Januvia, Onglyza, and Tradjenta
- increases incretin concentrations, insulin secretion, and decreases glucagon
- does not produce low blood sugar
Amylin Mimetic/Analog (Symlin)
- decreases glucagon secretion, slows gastric emptying, and causes weight loss
- can cause low blood sugar if used with insulin
Insulins

Rapid-Acting Insulin - Humalog
Short-Acting Insulin (Regular) - Humulin R
NPH Insulin - Humulin N, Lantus, Levemir - has no "peaks"
Insulin Mixtures - Humulin 70/30 (70% NPH, 30% regular or short-acting insulin)
Hopefully, this article provided a wealth of knowledge on the thyroid gland and diabetes. We haven't covered the anterior pituitary yet, so stay tuned in future articles discussing those target organs.